VESICOURETERAL REFLUX – SYMPTOMS, CAUSES, AND TREATMENT
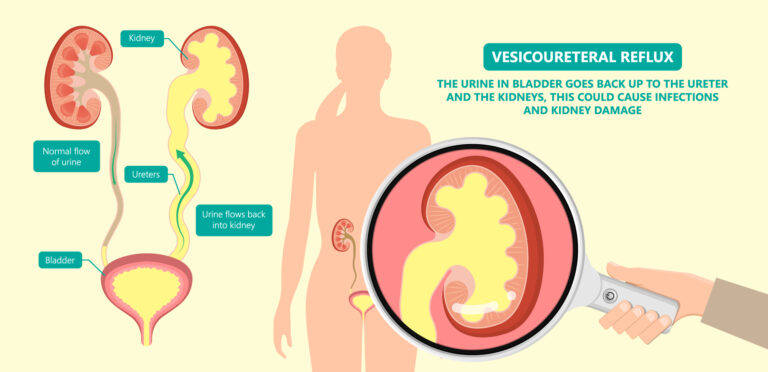
Vesicoureteral reflux is the abnormal flow of urine from your bladder back up the tubes (ureters) that join your kidneys to your bladder. Generally, urine flows from your kidneys through the ureters down to your bladder. It is not supposed to flow back up.
Vesicoureteral reflux is generally diagnosed in infants and children. The disorder increases the risk of urinary tract infections, which, if left untreated, could lead to kidney damage.
Children might outgrow primary vesicoureteral reflux. Treatment, which involves medication or surgery, aims at preventing kidney damage.
TYPES
- Hydronephrosis
SYMPTOMS
Urinary tract infections commonly happen in people with vesicoureteral reflux. A urinary tract infection (UTI) does not always cause noticeable signs and symptoms, though most people have some.
These signs and symptoms could include:
- A strong, continuous urge to urinate
- A burning feeling when urinating
- The requirement to pass small amounts of urine frequently
- Cloudy urine
- Fever
- Pain in your side (flank) or abdomen
A UTI might be difficult to diagnose in children, who might have only nonspecific signs and symptoms. Signs and symptoms in infants with a UTI might also include:
- An unexplained fever
- Lack of appetite
- Irritability
As your child gets older, untreated vesicoureteral reflux could lead to:
- Bed-wetting
- Constipation or loss of control over the bowel movements
- High blood pressure
- Protein in urine
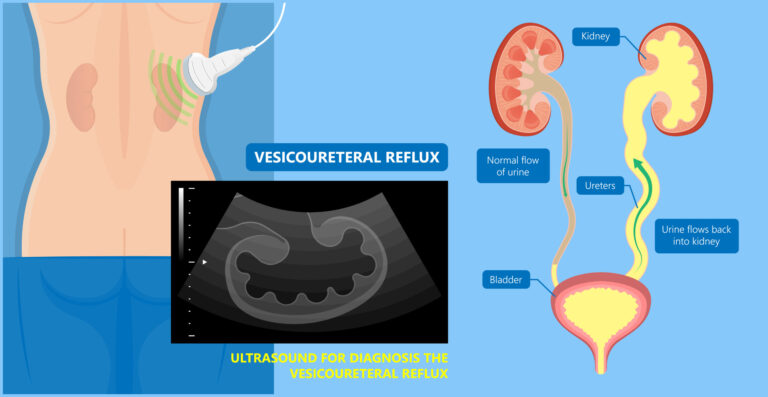
Another indication of vesicoureteral reflux, which might be detected before birth by sonogram, is swelling of the kidneys or the urine-collecting structures of one or both kidneys (hydronephrosis) in the fetus, caused by the backup of urine within the kidneys.
WHEN SHOULD YOU SEE A DOCTOR?
Contact your doctor immediately if your child develops any of the signs or symptoms of a UTI, like:
- A strong, continuous urge to urinate
- A burning feeling when urinating
- Abdominal or flank pain
Contact your doctor about fever if your child:
- Is younger than three months old and has a rectal temperature of 100.4 F (38 C) or higher
- Is three months or older and has a fever of 100.4 F (38 C) or higher and seems to be ill
- Is eating poorly or has had significant changes in mood
CAUSES
Your urinary system involves your kidneys, ureters, bladder, and urethra. All play a part in removing waste products from your body through urine.
Tubes known as ureters carry urine from your kidneys down to your bladder, where it is stored until it exits the body through another tube (the urethra) during urination.
Vesicoureteral reflux could develop in two types, primary and secondary:
- Primary vesicoureteral reflux – Children with primary vesicoureteral reflux are born with a defect in the valve that usually prevents urine from flowing backward from the bladder into the ureters. Primary vesicoureteral reflux is the most common type. As your child grows, the ureters lengthen and straighten, which might improve valve function and ultimately correct the reflux. This type of vesicoureteral reflux tends to run in families, which indicates that it might be genetic, but the exact cause of the defect is unknown.
- Secondary vesicoureteral reflux – The cause of this form of reflux is most often from the failure of the bladder to empty properly, either because of a blockage or failure of the bladder muscle or damage to the nerves that control regular bladder emptying.
RISK FACTORS
Risk factors for vesicoureteral reflux include:
People who might be more susceptible to gastroenteritis include:
- Bladder and bowel dysfunction (BBD) – Children with BBD hold their urine and stool and experience recurrent urinary tract infections, which could contribute to vesicoureteral reflux.
- Race – White children appear to have a greater risk of vesicoureteral reflux.
- Sex – Normally, girls have a much higher risk of having this condition than boys do. The exception is for vesicoureteral reflux that is present at birth, which is more common in boys.
- Age – Infants and children up to age two are more likely to have vesicoureteral reflux than older children are.
- Family history – Primary vesicoureteral reflux usually runs in families. Children whose parents had the condition are at greater risk of developing it. Siblings of children who have the condition also are at higher risk, so your doctor might recommend screening for siblings of a child with primary vesicoureteral reflux.
COMPLICATIONS
Kidney damage is the main concern with vesicoureteral reflux. The more severe the reflux, the more severe the complications are likely to be.
Complications might include:
- Kidney (renal) scarring – Untreated UTIs could lead to scarring, which is permanent damage to kidney tissue. Extensive scarring might lead to high blood pressure and kidney failure.
- High blood pressure – Because the kidneys remove waste from the bloodstream, damage to your kidneys and the resultant build-up of wastes could raise your blood pressure.
- Kidney failure – Scarring could cause a loss of function in the filtering part of the kidney. This might lead to kidney failure, which could happen quickly (acute kidney failure) or might develop over time (chronic kidney disease).
DIAGNOSIS
A urine test could reveal whether your child has a UTI. Other tests might be necessary, including:
- Kidney and bladder ultrasound – This imaging method uses high-frequency sound waves to produce pictures of the kidney and bladder. Ultrasound could detect structural abnormalities. This same technology often used during pregnancy to monitor fetal development, might also reveal swollen kidneys in the baby, an indication of primary vesicoureteral reflux.
- Specialized X-ray of urinary tract system – This test uses X-rays of the bladder when it is full and when it is emptying to detect abnormalities. A thin, flexible tube (catheter) is inserted through the urethra and into the bladder while your child lies down on his or her back on an X-ray table. After the contrast dye is administered into the bladder through the catheter, your child’s bladder is X-rayed in various positions.
Then the catheter is removed so that your child could urinate, and more X-rays are taken of the bladder and urethra during urination to see whether the urinary tract is functioning correctly. Risks related to this test include discomfort from the catheter or from having a full bladder and the possibility of a new urinary tract infection. - Nuclear scan – This test uses a tracer known as a radioisotope. The scanner detects the tracer and shows whether the urinary tract is functioning properly. Risks involve discomfort from the catheter and discomfort during urination.
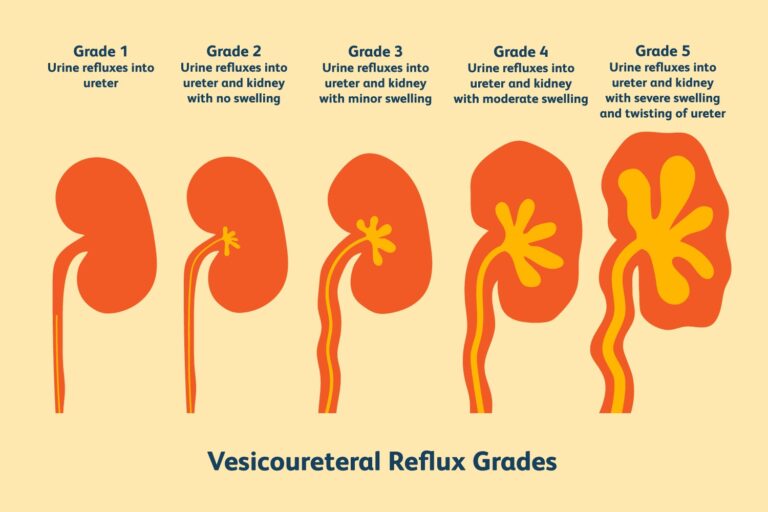
Grading the condition
After testing, doctors grade the degree of the reflux. In the mildest cases, the urine backs up only to the ureter (grade I). The most severe cases include severe kidney swelling (hydronephrosis) and twisting of the ureter (grade V).
TREATMENT
Treatment options for vesicoureteral reflux depend upon the severity of the condition. Children with mild cases of primary vesicoureteral reflux might ultimately outgrow the disorder. In this case, your doctor might recommend a wait-and-see approach.
For more severe vesicoureteral reflux, treatment options are:
Medications
UTIs require immediate treatment with antibiotics to keep the infection from moving to the kidneys. To prevent UTIs, doctors might also prescribe antibiotics at a lower dose than for treating an infection.
A child being treated with medication requires to be monitored for as long as he or she is taking antibiotics. This involves periodic physical examinations and urine tests to detect breakthrough infections — UTIs that happen despite the antibiotic treatment — and occasional radiographic scans of the bladder and kidneys to find out if your child has outgrown vesicoureteral reflux.
Surgery
Surgery for vesicoureteral reflux repairs the defect in the valve in between the bladder and each affected ureter. A defect in the valve keeps the valve from closing and prevents urine from flowing backward.
Methods of surgical repair include:
- Open surgery – Performed using general anesthesia, this surgery needs an incision in the lower abdomen through which the surgeon repairs the problem. This type of surgery generally needs a few days’ stays in the hospital, during which a catheter is kept in place to drain your child’s bladder. Vesicoureteral reflux might persist in a small number of children, but it usually resolves on its own without the need for further intervention.
- Robotic-assisted laparoscopic surgery – Similar to open surgery, this procedure includes repairing the valve between the ureter and the bladder, but it is performed using small incisions. Advantages involve smaller incisions and possibly fewer bladder spasms than open surgery.
But preliminary findings suggest that robotic-assisted laparoscopic surgery might not have as high of a success rate as open surgery. The procedure was also related to a longer operating time, but a shorter hospital stays. - Endoscopic surgery – In this procedure, the doctor inserts a lighted tube (cystoscope) through the urethra to see inside your child’s bladder, and then administers a bulking agent around the opening of the affected ureter to try to strengthen the valve’s ability to close properly.
This method is minimally invasive compared with open surgery and presents fewer risks, though it might not be as effective. This procedure also needs general anesthesia, but generally could be performed as outpatient surgery.
Treatment of vesicoureteral reflux at Specialty Care Clinics is unique in its individualized approach to medical care. Cases of reflux are not all the same. Specialty Care Clinics pediatric urologists emphasize a thorough medical history and examination to fit each patient and family.
Because bowel and bladder dysfunction could have a significant impact in some patients with recurring urinary tract infections with or without reflux, Specialty Care Clinics has a state-of-the-art pelvic floor rehabilitation and biofeedback program to help cure these conditions.
When surgery is necessary, your Specialty Care Clinics care team implements a surgical plan designed to give the best results with the least invasive method. Specialty Care Clinics physicians are innovators of the hidden incision endoscopic surgery (HIdES) procedure, which allows for surgery to be done with incisions that are not visible if the child wears a bathing suit.
If you or anyone you know is suffering from vesicoureteral reflux, our expert providers at Specialty Care Clinics will take care of your health and help you recover.
Call us on (469) 545-9983 to book an appointment with our specialists.
