KNOWING PERIPHERAL VASCULAR DISEASE
Peripheral vascular disease (PVD) is a blood course problem that causes the veins outside of your heart and cerebrum to be limited, square, or spasm. This can occur in your courses or veins. It causes limited blood flow to the arms, legs, or other body parts. It happens when courses or veins get smaller, become obstructed, or spasm.
PVD ordinarily causes pain and weakness, regularly in your legs, and particularly during exercise. The pain as a rule improves with rest.

IS THERE ANY RELATION BETWEEN ATHEROSCLEROSIS AND PERIPHERAL VASCULAR DISEASE?
Atherosclerosis is a continuous cycle by which hard cholesterol substances (plaques) are saved in the dividers of the arteries. This development of cholesterol plaques causes solidifying of the course dividers and restricts the internal channel (lumen) of the vein. At the point when this occurs in the peripheral dissemination, peripheral vascular disease is the outcome. The atherosclerosis cycle starts from the get-go throughout everyday life (as soon as adolescents in certain individuals). At the point when atherosclerosis is gentle and the arteries are not considered restricted, atherosclerosis causes no indications. Subsequently, numerous grown-ups ordinarily are uninformed that their arteries are step by step aggregating cholesterol plaques. Be that as it may, when atherosclerosis becomes progressed with maturing, it can cause basic occlusive disease of the arteries bringing about tissue ischemia (absence of blood and oxygen).
Arteries that are limited by cutting-edge atherosclerosis can cause diseases in various organs. For instance, progressed atherosclerosis of the coronary (arteries that supply heart muscles) can prompt angina, coronary illness, and cardiovascular failures. Progressed atherosclerosis of the carotid and cerebral (arteries that supply blood to the mind) can prompt strokes and transient ischemic assaults (TIA). Progressed atherosclerosis in the lower limits can prompt pain while strolling or working out (claudication), insufficient injury mending, as well as leg ulcers.
FACTORS LEADING TO PERIPHERAL VASCULAR DISEASE?
The most widely recognized reason for PVD is atherosclerosis, the development of plaque inside the supply route divider. Plaque decreases how much blood flows to the appendages. It additionally diminishes the oxygen and supplements accessible to the tissue. Blood clumps might frame on the vein dividers, further diminishing the inward side of the vein and squaring off significant arteries. Different reasons for PVD might include:
- Injury to the arms or legs
- Sporadic life structures of muscles or tendons
- Infection
- Individuals with coronary corridor disease (CAD) frequently additionally have PVD.

There are two types of PVD and the causes may differ based on types:
- Functional PVD: Your vessels normally extend and limit because of your current circumstance. But in functional PVD, your vessels misrepresent their reaction. Functional PVD can commonly be caused due to:
- Emotional stress,
- Cold temperatures,
- Operating vibrating machinery or tools, and
- Drugs.
- Organic PVD: Organic PVD implies there’s the adjustment of the construction of your veins. For instance, plaque development from arteriosclerosis can make your veins slender. The essential drivers of natural PVD are:
- Smoking,
- High blood pressure,
- Diabetes
- High cholesterol,
- Extreme injuries,
- Ligament or Muscles with abnormal structures,
- Blood vessel inflammation, and
- Infection.
If the peripheral vascular disease is not diagnosed and treated on time may lead to complications such as:
- Tissue death leading to limb amputation.
- Impotence.
- Pale skin.
- Pain at rest and with movement.
- Severe pain restricting mobility.
- Wounds that don’t heal.
HOW TO RECOGNIZE PERIPHERAL VASCULAR DISEASE?
Usually, many people suffering from peripheral artery disease have mild or no symptoms. But, some people may experience leg pain when walking referred to as claudication.
Some of the symptoms of claudication include muscle pain or cramping in your legs or arms. These may be triggered by activities, such as walking, but disappears after a few minutes of rest. The area of the pain relies upon the area of the stopped up or limited supply route.
The seriousness of claudication changes broadly, from gentle uneasiness to crippling pain. Extreme claudication can make it difficult for you to walk or do different kinds of actual work.
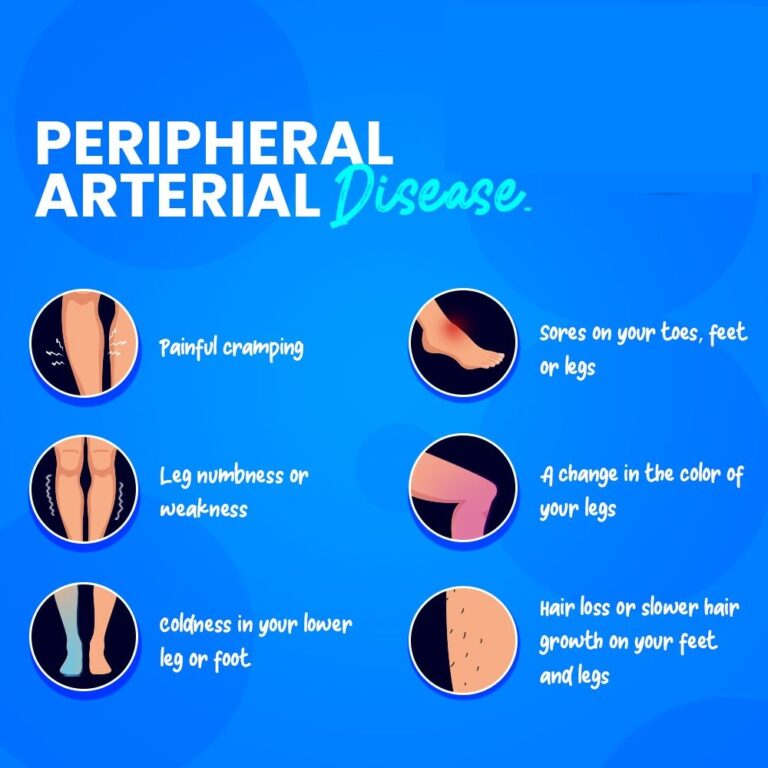
The signs and symptoms of peripheral artery disease include:
- Painful cramping in one or both of your hips, thighs, or calf muscles.
- The pain worsens after certain activities, such as walking or climbing stairs.
- Numbness or weakness in legs.
- Coldness in your lower leg or foot.
- Sores on your toes, feet, or legs that won’t heal.
- A change in the color of your legs.
- Hair loss or slower hair growth on your feet and legs.
- Slower growth of your toenails.
- Shiny skin on your legs
- No pulse or a weak pulse in your legs or feet.
- Erectile dysfunction in men.
- Pain when using your arms.
Aching and cramping worsen in arms during activities such as knitting, writing, or doing other manual tasks.
WHAT ARE THE RISK FACTORS OF PERIPHERAL VASCULAR DISEASE?
Peripheral vascular disease is more normal in men than in ladies and most frequently happens in older people (beyond 50 years old). The risk factors for peripheral vascular disease are those that incline toward the improvement of atherosclerosis. You are at high risk of developing the peripheral vascular disease if you have:
- High blood cholesterol,
- Low blood levels of the “good” HDL cholesterol,
- Cigarette smoking,
- Diabetes mellitus (both type 1 and type 2 diabetes),
- High blood pressure or a family history of hypertension,
- A family history of atherosclerotic disease,
- Chronic renal failure,
- Overweight or obesity, and
- Physical inactivity.
HOW TO TREAT PERIPHERAL VASCULAR DISEASE?
The treatment of PVD includes:
- Stopping the disease from progressing,
- Help you manage your pain,
- Reduce other symptoms so you can remain active, and
- Lower your risk for serious complications.

First-line treatment commonly includes a way of life adjustments. Your doctor will propose a standard exercise program that incorporates strolling, a fair eating routine and getting thinner.
If you smoke, you ought to stop. Smoking straightforwardly causes the diminished blood flow in vessels. It likewise makes PVD deteriorate, as well as increases your risk of respiratory failure and stroke.
Medication is required for lifestyle changes alone isn’t enough. These may include:
- Medicine to increase blood flow and relieve symptoms of claudication.
- Medicine to reduce blood clotting.
- Medicine to lower high cholesterol.
- Medicine to lower high blood pressure.
- Medication to control blood sugar.
Surgery may include angioplasty or vascular surgery to remove significant artery blockages. Vascular surgery allows for blood to bypass the narrow area through vein grafting.
OUTLOOK
A lifestyle change will be effective to treat PVD if diagnosed early. You will be able to feel improvement if you can walk without pain. Talk to your doctor if you experience symptoms of PVD.
If you or anyone you know is suffering from peripheral vascular disease, our expert providers at Specialty Care Clinics will take care of your health and help you recover.
Call us on (469) 545-9983 to book an appointment with our specialists.
