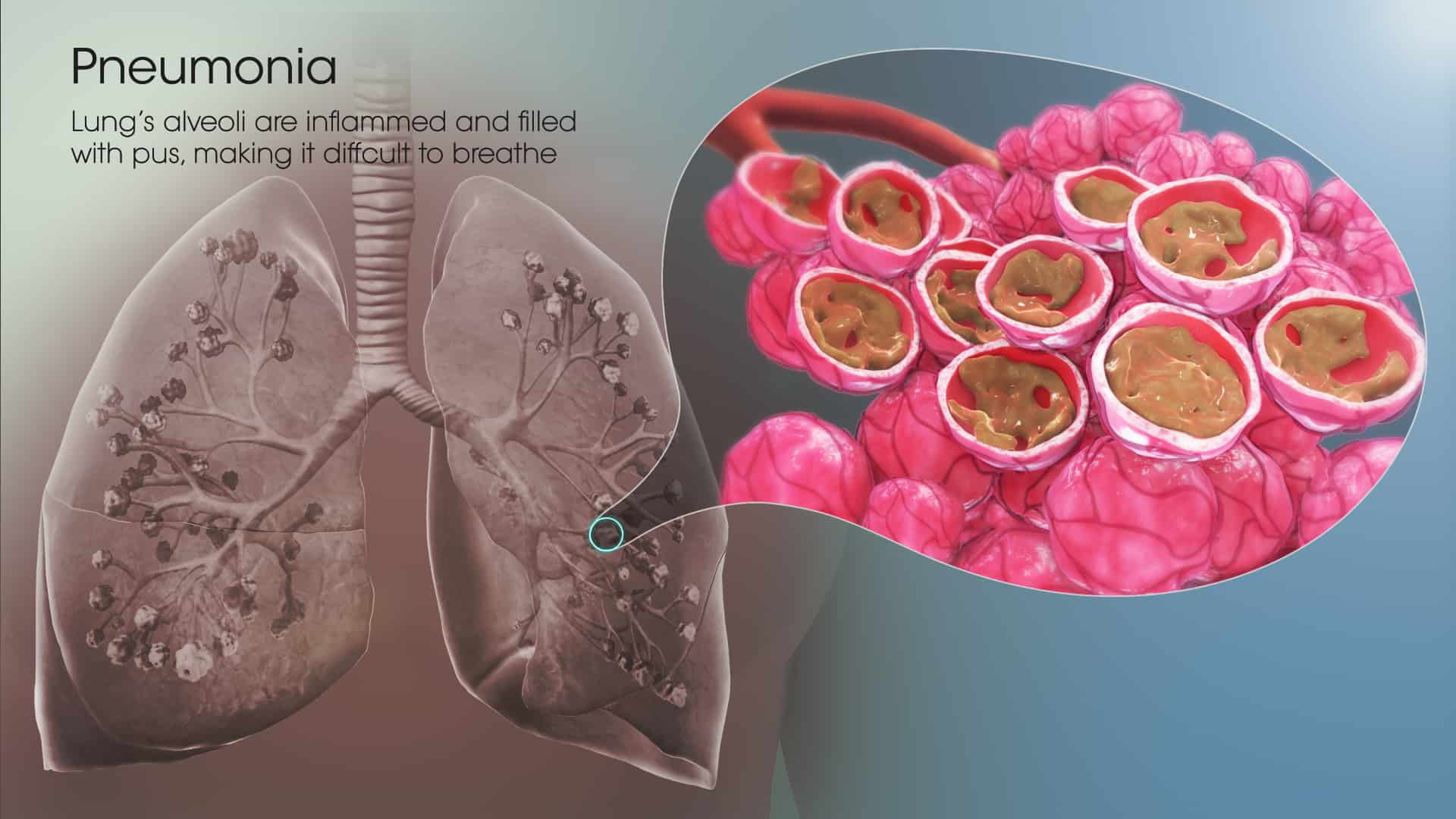
What is Pneumonia?
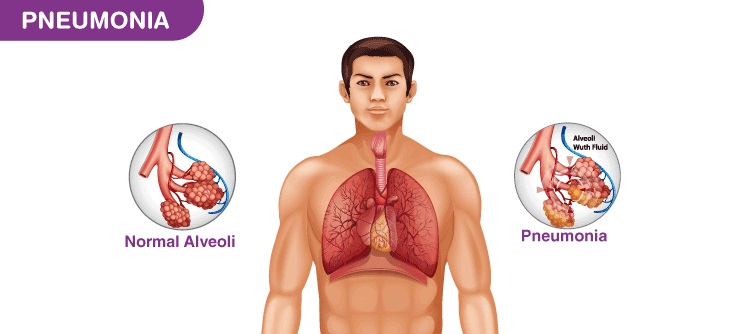
Pneumonia is an infection that aggravates the air sacs in one or both lungs. The air sacs might fill with fluid or pus (purulent material), causing cough with phlegm or pus, fever, chills, and difficulty breathing. A variety of organisms, including bacteria, viruses, and fungi, could cause pneumonia.
Pneumonia could range in seriousness from mild to life-threatening. It is most severe for infants and young children, people older than age 65, and people with health problems or weakened immune systems.
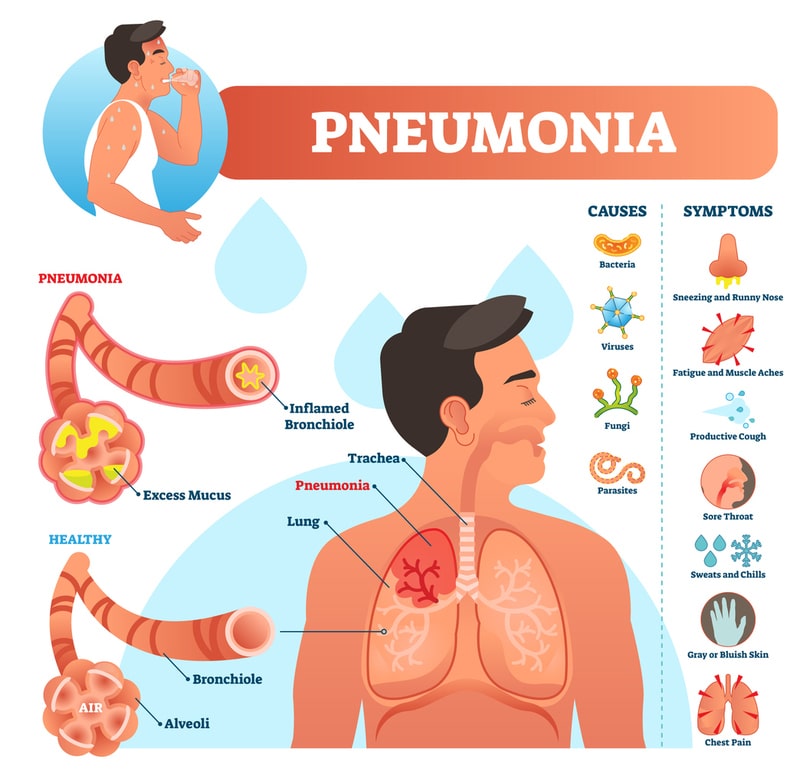
Pneumonia Symptoms
The signs and symptoms of pneumonia vary from mild to severe, depending on factors like the type of germ causing the infection, and your age and overall health. Mild signs and symptoms often are the same as those of a cold or flu, but they last longer.
Signs and symptoms of pneumonia might include:
- Chest pain when you breathe or cough
- Confusion or changes in mental awareness (for adults age 65 and older)
- Cough, which might produce phlegm
- Fatigue
- Fever, sweating, and shaking chills
- Lower than normal body temperature (for adults older than age 65 and people with weak immune systems)
- Nausea, vomiting, or diarrhea
- Shortness of breath
Newborns and infants may not display any sign of the infection. Or they might vomit, have a fever and cough, appear restless, tired, and without energy, or have difficulty breathing and eating.
When should you see a doctor?
See your doctor if you have difficulty breathing, chest pain, persistent fever of 102 F (39 C) or higher, or persistent cough, particularly if you are coughing up the pus.
It is particularly important that people in these high-risk groups see a doctor:
- Adults older than age 65
- Children younger than age two with signs and symptoms
- People who have an underlying health condition or a weakened immune system
- People receiving chemotherapy or taking medicines that suppress the immune system
For some older adults and people with heart failure or chronic lung problems, pneumonia could quickly become a life-threatening condition.
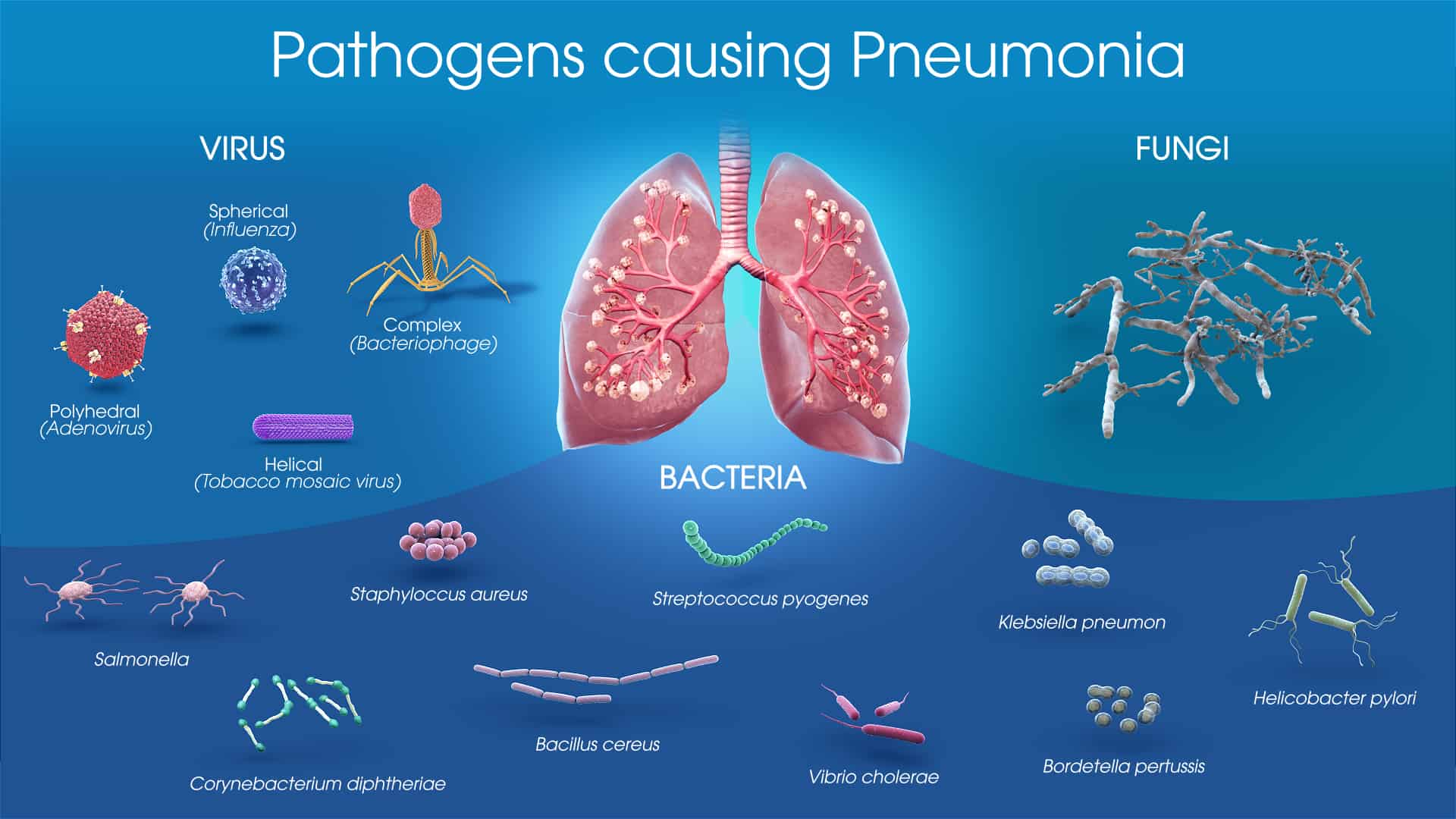
Pneumonia Causes
Many germs could cause pneumonia. The most frequent are bacteria and viruses in the air we breathe. Your body often prevents these germs from infecting your lungs. But sometimes these germs could overpower your immune system, even if your health is generally good.
Pneumonia is classified based on the types of germs that cause it and where you got the infection.
Community-acquired pneumonia
Community-acquired pneumonia is the most frequent type of pneumonia. This happens outside of hospitals or other healthcare facilities. It might be caused by:
- Bacteria – The most frequent cause of bacterial pneumonia in the U.S. is Streptococcus pneumoniae. This type of pneumonia could happen on its own or after you have had a cold or the flu. It may affect one part (lobe) of the lung, a condition known as lobar pneumonia.
- Bacteria-like organisms – Mycoplasma pneumoniae also could cause pneumonia. It usually produces milder symptoms compared to other types of pneumonia. Walking pneumonia is an informal name given to this type of pneumonia, which generally is not severe enough to need bed rest.
- Fungi – This type of pneumonia is most common in people with chronic health issues or weakened immune systems, and in people who have inhaled large doses of the organisms. The fungi that cause it could be found in soil or bird droppings and vary depending upon geographic location.
- Viruses, including COVID-19 – Some of the viruses that cause colds and the flu could cause pneumonia. Viruses are the most frequent cause of pneumonia in children younger than five years. Viral pneumonia is generally mild. But in some cases, it could become very severe. Coronavirus 2019 (COVID-19) might cause pneumonia, which can become severe.
Hospital-acquired pneumonia
Some people catch pneumonia during a hospital stay for another disease. Hospital-acquired pneumonia can be severe because the bacteria causing it might be more resistant to antibiotics and because the people who get it are already sick. People who are on breathing machines (ventilators), usually used in intensive care units, are at higher risk of this type of pneumonia.
Health care-acquired pneumonia
Health care-acquired pneumonia is a bacterial infection that happens in people who live in long-term care facilities or who receive care in outpatient clinics, including kidney dialysis centers. Like hospital-acquired pneumonia, healthcare-acquired pneumonia could be caused by bacteria that are more resistant to antibiotics.
Aspiration pneumonia
Aspiration pneumonia happens when you inhale food, drink, vomit, or saliva into your lungs. Aspiration is more likely if something disturbs your normal gag reflex, like a brain injury or swallowing problem, or excessive use of alcohol or drugs.
Pneumonia Risk factors
Pneumonia could affect anyone. But the two age groups at greatest risk are:
Children up to two years old or younger
People who are age 65 or older
Other risk factors include:
- Being hospitalized – You are at higher risk of pneumonia if you are in a hospital intensive care unit, particularly if you are on a machine that helps you breathe (a ventilator).
- Chronic disease – You are more likely to get pneumonia if you suffer from asthma, chronic obstructive pulmonary disease (COPD), or heart disease.
- Smoking – Smoking harms your body’s natural defenses against the bacteria and viruses that cause pneumonia.
- Weakened or suppressed immune system – People who have HIV/AIDS, who have had an organ transplant, or who receive chemotherapy or long-term steroids are at risk.
Pneumonia Complications
Even with treatment, some people with pneumonia, particularly those in high-risk groups, might experience complications, including:
- Bacteria in the bloodstream (bacteremia) – Bacteria that enter the bloodstream from your lungs could spread the infection to other organs, potentially causing organ failure.
- Difficulty breathing – If your pneumonia is severe or you have chronic underlying lung diseases, you might have trouble breathing in enough oxygen. You might need to be hospitalized and use a breathing machine (ventilator) while your lung heals.
- Fluid accumulation around the lungs (pleural effusion) – Pneumonia might cause fluid to build up in the thin space between layers of tissue that line the lungs and chest cavity (pleura). If the fluid becomes infected, you might need to have it drained through a chest tube or removed with surgery.
- Lung abscess – An abscess happens if pus forms in a cavity in the lung. An abscess is generally treated with antibiotics. At times, surgery or drainage with a long needle or tube placed into the abscess is required to remove the pus.
Pneumonia Prevention
To help prevent pneumonia:
- Get vaccinated – Vaccines are available to prevent a few types of pneumonia and the flu. Speak with your doctor about getting these shots. The vaccination guidelines have changed over time so be sure to review your vaccination status with your doctor even if you recall previously receiving a pneumonia vaccine.
- Make sure children get vaccinated – Doctors recommend a different pneumonia vaccine for children younger than age two and for children ages two to five years who are at particular risk of pneumococcal disease. Children who attend a group childcare center should also receive the vaccine. Doctors also recommend flu shots for children older than six months.
- Practice good hygiene – To protect yourself against respiratory infections that at times lead to pneumonia, wash your hands regularly or use an alcohol-based hand sanitizer.
- Do not smoke – Smoking harms your lungs’ natural defenses against respiratory infections.
Keep your immune system strong – Get enough sleep, exercise daily, and eat a healthy diet.
Pneumonia Diagnosis
Your doctor will begin by asking about your medical history and doing a physical examination, including listening to your lungs with a stethoscope to check for abnormal bubbling or crackling sounds that indicate pneumonia.
If pneumonia is suspected, your doctor might recommend the following tests:
- Blood tests – Blood tests are used to verify an infection and to try to identify the type of organism causing the infection. However, exact identification is not always possible.
- Chest X-ray – This helps your doctor diagnose pneumonia and determine the extent and place of the infection. However, it cannot tell your doctor what kind of germ is causing pneumonia.
- Pulse oximetry – This measures the oxygen level in your bloodstream. Pneumonia could prevent your lungs from moving enough oxygen into your bloodstream.
- Sputum test – A sample of fluid from your lungs (sputum) is taken after a deep cough and analyzed to help identify the cause of the infection.
Your doctor may order additional tests if you are older than age 65, are in the hospital, or have severe symptoms or health conditions. These might include:
- CT scan – If your pneumonia is not clearing as quickly as expected, your doctor might recommend a chest CT scan to get a more detailed image of your lungs.
- Pleural fluid culture – A fluid sample is taken by putting a needle between your ribs from the pleural region and analyzed to help determine the type of infection.
Pneumonia Treatment
The treatment for pneumonia consists of curing the infection and preventing complications. People who have community-acquired pneumonia usually could be treated at home with medication. Although most symptoms ease in a few days or weeks, the feeling of tiredness could persist for a month or more.
Specific treatments depend upon the type and severity of your pneumonia, your age, and your overall health. The options include:
- Antibiotics – These medications are used in the treatment of bacterial pneumonia. It might take time to identify the type of bacteria causing your pneumonia and to choose the best antibiotic to treat it. If your symptoms do not improve, your doctor might recommend a different antibiotic.
- Cough medicine – This medicine might be used to calm your cough so that you could rest. Because coughing helps loosen and move fluid from your lungs, it is a good idea not to remove your cough completely. In addition to this, you should know that very few studies have looked at whether over-the-counter cough medicines lessen coughing caused by pneumonia. If you want to try a cough suppressant, use the lowest dose to help you get some rest.
- Fever reducers/pain relievers – You might take these as needed for fever and discomfort. These involve drugs like aspirin, ibuprofen (Advil, Motrin IB, others), and acetaminophen (Tylenol, others).
Hospitalization
You might need to be hospitalized if:
- You are older than age 65
- You are confused about the time, the people, or the places
- Your kidney function has declined
- Your systolic blood pressure is below 90 millimeters of mercury (mm Hg) or your diastolic blood pressure is equal to 60 mm Hg or below
- Your breathing is quick (30 breaths or more per minute)
- You need breathing assistance
- Your temperature is below normal
- Your heart rate is less than 50 or more than 100
You might be admitted to the intensive care unit if you need to be placed on a breathing machine (ventilator) or if your symptoms are severe.
Children might be hospitalized if:
- They are younger than age two months
- They are lethargic or excessively sleepy
- They have trouble breathing
- They have low blood oxygen levels
- They appear dehydrated
If you or anyone you know is suffering from pneumonia, our expert providers at Specialty Care Clinics will take care of your health and help you recover.
Call 469-545-9983 to book a telehealth appointment for an at-home check-up.