WHAT IS GIANT CELL ARTERITIS?
Giant cell arteritis is an inflammation (swelling) of the lining of your arteries. Most often, it affects the arteries in your head, particularly those in your temples. For this reason, giant cell arteritis is otherwise known as temporal arteritis.
Giant cell arteritis commonly causes headaches, scalp tenderness, jaw pain, and vision issues. Untreated, it could lead to blindness.
Prompt treatment with corticosteroid medications generally eases symptoms of giant cell arteritis and may prevent loss of vision. You will likely start to feel better within days of beginning treatment. But even with treatment, relapses are frequent.
You will require to visit your doctor or primary care physician regularly for check-ups and treatment of any side effects from taking corticosteroids.
GIANT CELL ARTERITIS SYMPTOMS
The most common symptoms of giant cell arteritis are head pain and tenderness usually severe that generally affects both temples. Head pain could progressively get worse, come and go, or subside momentarily.
Usually, signs and symptoms of giant cell arteritis include:
- Continuous, severe head pain, generally in your temple area
- Scalp tenderness
- Pain to the jaw when chewing or opening the mouth
- Fever
- Fatigue
- Unintended weight loss
- Vision loss or double vision, especially in people who also have jaw pain
- Unexpected, permanent loss of vision in one eye

Pain and stiffness in the neck, shoulders, or hips are common symptoms of an associated disorder, polymyalgia rheumatica. About fifty percent of people with giant cell arteritis also suffer from polymyalgia rheumatica.
WHEN SHOULD YOU SEE A DOCTOR?
If you develop a new, continuous headache or any of the signs and symptoms listed above, see your doctor or primary care physician without delay. If you are diagnosed with giant cell arteritis, beginning treatment as soon as possible could generally help prevent vision loss.
 GIANT CELL ARTERITIS CAUSES
GIANT CELL ARTERITIS CAUSES
With giant cell arteritis, the lining of arteries becomes inflamed (swollen), causing them to swell. This inflammation narrows your blood vessels, lowering the amount of blood and, therefore, oxygen and vital nutrients that reach your body’s tissues.
Almost any large or medium-sized artery could be affected, but inflammation most usually happens in the arteries in the temples. These are right in front of your ears and continue upwards through your scalp.
What causes these arteries to become inflamed (swollen) is not known, but it is thought to involve abnormal attacks on artery walls by the immune system. Specific genes and environmental factors may increase your vulnerability to the condition.
GIANT CELL ARTERITIS RISK FACTORS
Various factors could increase your risk of developing giant cell arteritis, including:
- Age –Giant cell arteritis affects adults only, and rarely those under 50 years. Most people with this condition develop signs and symptoms between the ages of 70 years and 80 years.
- Sex –Women are about twice as susceptible to developing the disease as men.
- Race and geographic region –Giant cell arteritis is most frequent among white people in Northern European populations or of Scandinavian descent.
- Polymyalgia rheumatic –Having polymyalgia rheumatica puts you at high risk of developing giant cell arteritis.
- Family history –Sometimes the condition runs in the families.
GIANT CELL ARTERITIS COMPLICATIONS
Giant cell arteritis could cause severe complications, including:
- Blindness –Reduced blood flow to your eyes could cause unexpected, painless vision loss in one or, rarely, both eyes. Loss of vision is generally permanent.
- Aortic aneurysm –An aneurysm is a protrusion that forms in a weakened blood vessel, generally in the large artery that runs down the center of your chest and abdomen (aorta). An aortic aneurysm may burst, causing life-threatening internal bleeding. Because this complication could happen even years after the diagnosis of giant cell arteritis, your doctor or primary care physician may monitor your aorta with annual chest X-rays or other imaging tests, for example, ultrasound and computed tomography (CT).
- Stroke –This is an unusual complication of giant cell arteritis.
GIANT CELL ARTERITIS DIAGNOSIS
Giant cell arteritis could be difficult to diagnose because its early symptoms resemble those of other common conditions. For this reason, your doctor or primary care physician will try to rule out other possible causes of your problem.
In addition to asking about your symptoms and medical history, your doctor or primary care physician is likely to perform a thorough physical examination, paying particular attention to your temporal arteries. Usually, one or both of these arteries are tender, with a lowered pulse and a hard, cordlike feel and appearance.
Your doctor or primary care physician may also suggest specific tests.
Blood tests
The following tests may be used to help diagnose your condition and to track your progress during treatment.
- Erythrocyte sedimentation rate – Commonly known as the sed rate, this test measures how quickly red blood cells fall to the base of a tube of blood. Red cells that drop quickly may indicate inflammation (swelling) in your body.
- C-reactive protein (CRP) – This measures a substance your liver produces when inflammation (swelling) is present.
Imaging tests
These may be used to diagnose giant cell arteritis and to monitor your response to treatment. Tests may include:
- Doppler ultrasound – This test uses sound waves to produce pictures of blood flowing through your blood vessels.
- Magnetic resonance angiography (MRA) – This test combines magnetic resonance imaging (MRI) with the use of a contrast material that produces detailed pictures of your blood vessels. Let your doctor or primary care physician know ahead of time if you are uncomfortable being confined in a small space because the test is conducted in a tube-shaped machine.
- Positron emission tomography (PET) – If your doctor or primary care physician suspects you may have giant cell arteritis in large arteries, for example, your aorta, he or she may suggest positron emission tomography (PET). This test uses an intravenous tracer solution that contains a small amount of radioactive material. A positron emission tomography (PET) scan can produce detailed pictures of your larger blood vessels and highlight areas of inflammation (swelling).
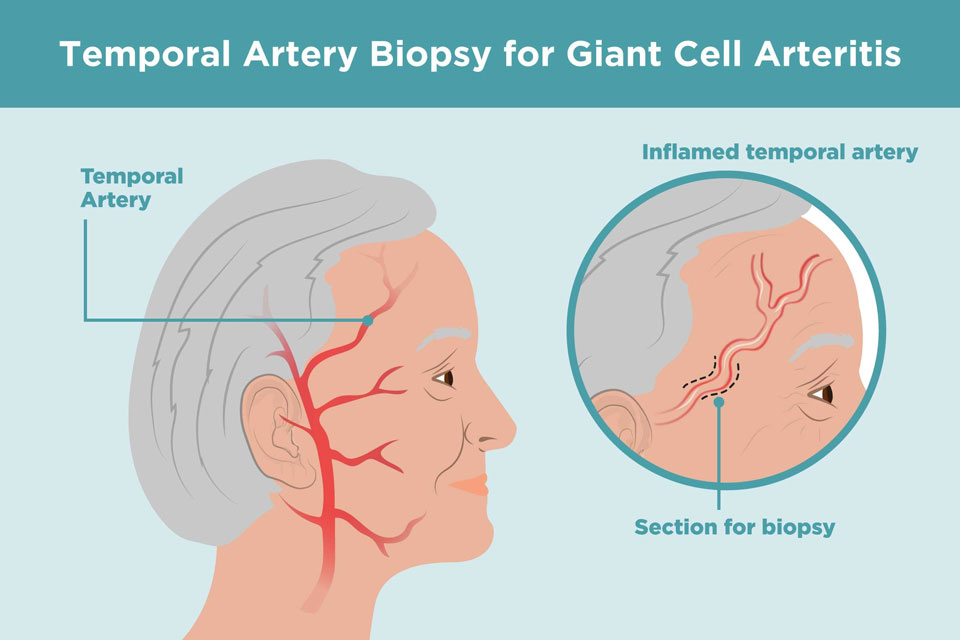
Giant cell arteritis Biopsy
The best way to verify a diagnosis of giant cell arteritis is by taking a tiny sample (biopsy) of the temporal artery. This artery is located close to the skin right in front of your ears and continues upwards through your scalp. The procedure is performed on an outpatient basis using local anesthesia, generally with little discomfort or scarring. The sample is analyzed under a microscope in a lab.
If you have giant cell arteritis, the artery will usually show inflammation that includes abnormally large cells, called giant cells, which give the disease its name. It is possible to have giant cell arteritis and have a negative biopsy result.
If the results are not clear, your doctor or primary care physician may advise another temporal artery biopsy on the other side of your head.
GIANT CELL ARTERITIS TREATMENT
The main treatment for giant cell arteritis comprises high doses of a corticosteroid drug for example prednisone. Because immediate treatment is required to prevent vision loss, your doctor or primary care physician is likely to begin medication even before confirming the diagnosis with a biopsy.
You will likely start to feel better within a few days of starting treatment. If you have a visual loss before beginning treatment with corticosteroids, it is unlikely that your vision will improve. Although, your unaffected eye may be able to compensate for some of the visual changes.
You might require to continue taking medication for one to two years or longer. After the first month, your doctor or primary care physician may slowly start to lower the dosage until you reach the lowest dose of corticosteroids required to control inflammation (swelling).
 Some symptoms, especially headaches, might return during this tapering period. This is the point of time at which many people also develop symptoms of polymyalgia rheumatica. Such flares could generally be treated with slight increases in the corticosteroid dose. Your doctor or primary care physician may also recommend an immune-suppressing drug known as methotrexate (Trexall).
Some symptoms, especially headaches, might return during this tapering period. This is the point of time at which many people also develop symptoms of polymyalgia rheumatica. Such flares could generally be treated with slight increases in the corticosteroid dose. Your doctor or primary care physician may also recommend an immune-suppressing drug known as methotrexate (Trexall).
Corticosteroids could lead to severe side effects, for example, osteoporosis, high blood pressure, and muscle weakness. To counter potential side effects, your doctor or primary care physician is likely to monitor your bone density and may prescribe calcium and vitamin D supplements or other medications to help stop bone loss.
The Food and Drug Administration (FDA) recently approved tocilizumab (Actemra) to treat giant cell arteritis. It is given as an injection under your skin. Side effects include making you more vulnerable to infections. More research is required.
If you or anyone you know is suffering from giant cell arteritis, our expert providers at Specialty Care Clinics will take care of your health and help you recover.
Call 469-545-9983 to book an telehealth appointment for an at home check-up.
