WHAT IS CALCIPHYLAXIS?
Calciphylaxis is a severe, unusual disease in which calcium accumulates in small blood vessels of the fat and skin tissues.
Calciphylaxis causes blood clots, painful skin ulcers and might cause severe infections that could lead to death. People who have calciphylaxis generally have kidney failure and are on dialysis or have had a kidney transplant. The condition could also happen in people without kidney disease.
CALCIPHYLAXIS SYMPTOMS
Signs and symptoms of calciphylaxis involve:
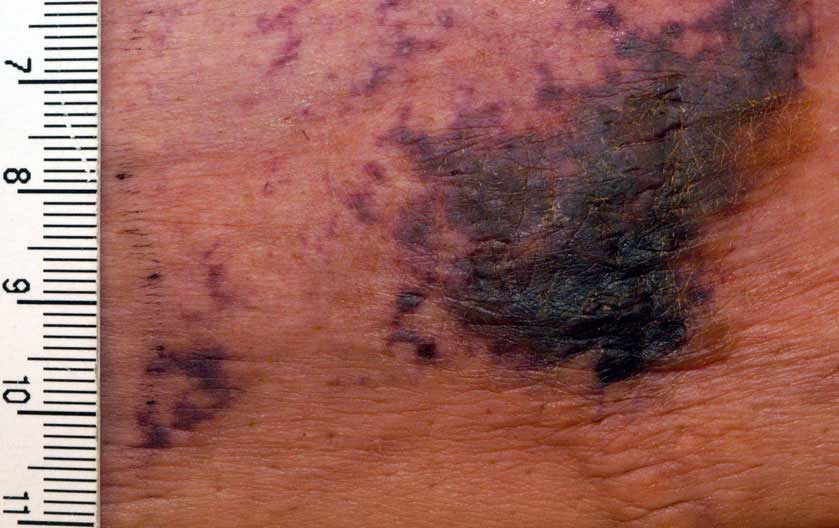
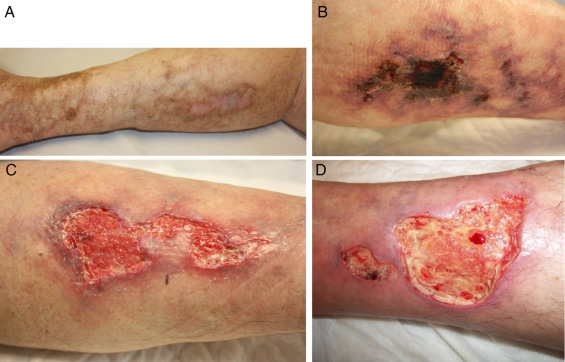
- Large purple net-like patterns on the skin
- Deep, very painful lumps that ulcerate creating open sores with a black-brown crust that fails to recover generally in skin regions with high-fat content, for example, the stomach and thigh, however, they could happen anywhere
- Infections from wounds that do not heal
CALCIPHYLAXIS CAUSES
The exact cause of calciphylaxis is not known, but recent studies have revealed that most people with the condition have abnormalities in blood-clotting factors. Blood-clotting factors are substances in your blood that help prevent bleeding. These abnormalities could lead to small blood clots forming more often than they generally would.
In addition to this, people with calciphylaxis have an imbalance in the metabolism of calcium. This causes calcium to be deposited in the smallest parts of the arteries (arterioles), which ultimately leads to the formation of blood clots in the arterioles. Blood clots could cause fat tissues and skin to be short of oxygen and nourishment.
CALCIPHYLAXIS RISK FACTORS
Calciphylaxis most commonly affects people who have last-stage kidney failure. Potential risk factors include:
- Being female
- Obesity
- Diabetes
- Abnormalities in blood-clotting factors
- Long-term dialysis and sometimes kidney transplantation
- An imbalance of calcium, phosphorus, and aluminum in the body
- Some medications, for example, warfarin (Coumadin, Jantoven), calcium-binding agents, or corticosteroids
- Overproduction of parathyroid hormone (PTH), which regulates the level of calcium and phosphorus in the body a condition otherwise known as hyperparathyroidism
- Uremia, a toxic condition in which substances generally eliminated in the urine for example calcium and phosphorus build up in the body
CALCIPHYLAXIS COMPLICATIONS
Complications of calciphylaxis include:
- Serious pain
- Large, deep, non-healing ulcers
- Blood infections
- Death, generally because of infection and multi-organ failure
Generally, the outlook for people with calciphylaxis is not hopeful. Early detection and treatment are very crucial in helping to stop severe infections.
CALCIPHYLAXIS DIAGNOSIS
To determine if you have calciphylaxis, your doctor or primary care physician will review your medical history, evaluate your symptoms and do a physical examination. Tests might include:
- Skin biopsy – To diagnose calciphylaxis, your doctor or primary care physician might remove a small tissue specimen from a region of damaged skin for examination.
- Blood tests – Blood specimens measure an assortment of substances in your blood calcium, phosphorus, parathyroid hormone, anomalies in blood-clotting or coagulation factors, aluminum, urea nitrogen, creatinine, and albumin, among others help your doctor or primary care physician evaluate your kidney and liver function.
- Imaging studies – X-rays might show branch-like calcium deposits in the blood vessels (vascular calcifications) that are normal in calciphylaxis and in other advanced kidney illnesses.
 CALCIPHYLAXIS TREATMENT
CALCIPHYLAXIS TREATMENT
Multiple interventions or procedures are used to treat calciphylaxis, including:
Restoration of oxygen and blood flow into the skin
Medication that helps keep your blood from clotting (anticoagulation medication) for example apixaban (Eliquis) will likely be prescribed to restore blood flow to damaged tissues.
Hyperbaric oxygen therapy could help to increase oxygen supply to the affected parts of the body. Or your doctor or primary care physician might use a low-dose tissue plasminogen activator (TPA) to dissolve blood clots in the small blood vessels of the skin.
Decreasing calcium deposits
- Dialysis – Your doctor or primary care physician might change your dialysis prescription if you are on kidney dialysis, including the medications used and the frequency of your dialysis.
- Changing medications – Your doctor or primary care physician will assess your current medications and eliminate potential triggers for calciphylaxis, for example, warfarin, corticosteroids, or iron, and might modify the amount (dose) of your calcium or vitamin D supplements.
- Taking medications – A medication known as sodium thiosulfate could decrease calcium build-up in the arterioles. It is given intravenously three times a week, generally during dialysis. Your doctor or primary care physician might also recommend a medication known as cinacalcet (Sensipar), which could help control parathyroid hormone (PTH). Other medications might be used to improve the balance of calcium and phosphorus.
- Surgery – If an overactive parathyroid gland (hyperparathyroidism) contributes to abnormal calcium metabolism by producing too much parathyroid hormone (PTH), surgery to remove all or part of the parathyroid glands might be suggested.

Applying intensive wound treatment
For sores to recover, some of the tissue affected by calciphylaxis might require to be surgically removed (debridement). In some cases, tissue could be removed using other methods, for example, wet dressings. Antibiotic treatment is part of treating and stopping wound infection.
You might be offered medication for managing pain because of calciphylaxis or during wound care.
If you or anyone you know is suffering from calciphylaxis, our expert providers at Specialty Care Clinics will take care of your health and help you recover.
Call 469-545-9983 to book an telehealth appointment for an at home check-up.
