CHARCOT FOOT AND DIABETES
Diabetes affects almost 6% of the population in the United States or about 16 million people. Diabetic Charcot foot syndrome is a rare and serious complication. Charcot foot or Charcot arthropathy affects people with peripheral neuropathy and diabetes mellitus. It is a limb-threatening lower-extremity complication of diabetes.
Diabetes is a serious condition of elevated blood sugar. Diabetic foot problems are a major health concern and might lead to hospitalization. Charcot’s foot affects the joints, bones, and soft tissues of the ankle or foot.
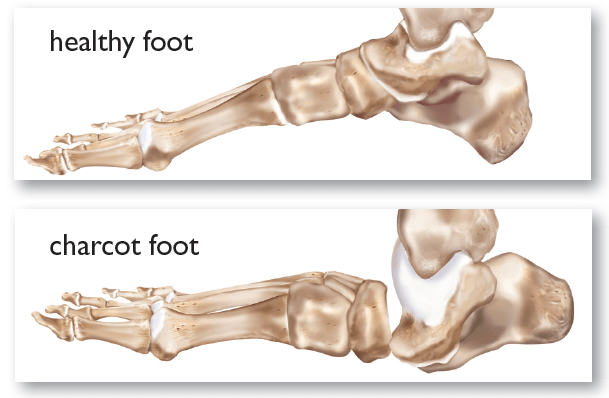
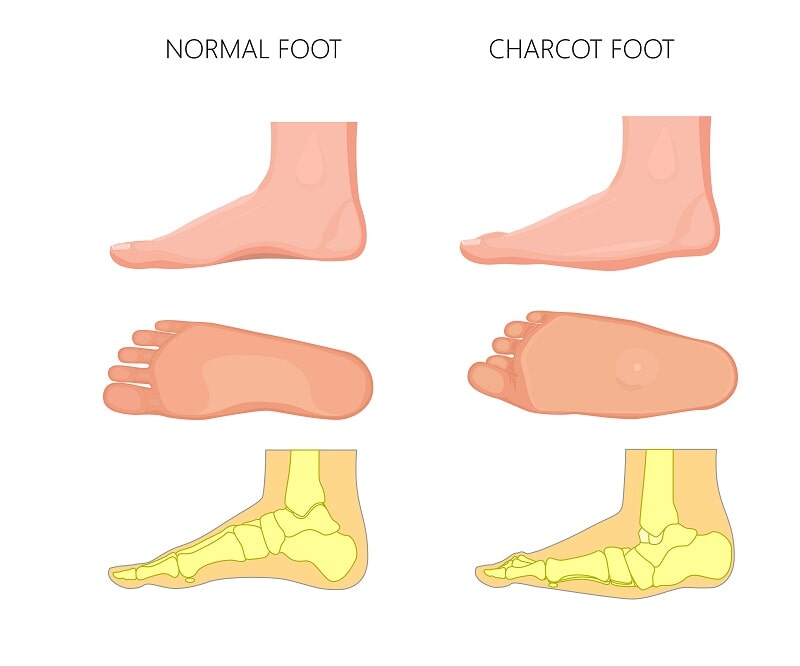
The bones of the foot become weak in this condition and can break. This can lead to the joints in the foot or ankle dislocating. The joints in the foot collapse and the foot becomes deformed if this is not diagnosed in its earliest stage.
Eventually, pressure sores develop in the foot or ankle due to a deformed foot. This causes open wounds leading to infection and amputation.

CAUSE OF CHARCOT FOOT
Neuropathy is the main cause of developing Charcot’s foot. This decreases the sensation and the ability to feel temperature, pain, or trauma. This is a common problem among diabetic people. Neuropathy or nerve damage diminishes the sensation of pain, injury, or trauma increases the risk of developing Charcot’s foot. Additionally, neuropathic patients suffering from a tight Achilles tendon have a tendency to develop Charcot foot.
Broken bone or injury in the foot, if not treated on time can worsen the deformity leading to foot sores and infection. Charcot’s foot is one of the major complications after organ transplantation in patients with diabetes.
The arch collapses as the mid-foot is involved in the Charcot foot, which rounds the bottom of the foot. This is referred to as rocker-bottom foot deformity. The toes might also start to curve under claws or ankles depending on the location of the bone break, leading to deformed and unstable feet.
Nerve damage or neuropathy is a diabetic complication leading to a loss of sensation in the feet. People suffering from diabetes sometimes can no longer feel irritation or even punctured skin. A small wound such as a blister can progress to a serious infection in a matter of days.
Diabetes causes damage to blood vessels that would decrease the blood flow to the feet. The bones become weak due to poor circulation and can cause disintegration of the bones and joints in the foot and ankle. People with diabetes are at high risk for breaking bones in the feet.
Diabetic patients may not realize when a bone fractures in the foot, because of nerve damage. They would continue to walk on the injured foot. This would lead to more severe fractures and joint dislocations. Sharp edges of broken bone within the foot would point downward toward the ground. This would increase the risk of chronic foot sores from the abnormal pressure on the foot.
Bone disintegration and trauma can warp and deform the shape of the foot. This is known as Charcot arthropathy. This is one of the most serious foot problems that diabetics face.
SYMPTOMS OF CHARCOT FOOT
Charcot arthropathy has other symptoms including pain such as:
- Swelling of the foot occurring without an obvious injury.
- Redness of the foot might occur in the early stages.
- The swelling, redness of the foot
- Warmth to the touch (the affected foot feels warmer than the other
- Changes to the bone visible in x-ray

The swelling and redness are often confused with bone infection. But, bone infection is unlikely if the skin is intact and there is no ulcer present.
DIAGNOSING CHARCOT FOOT
- Medical History and Physical Examination
The Podiatrist will discuss your general health and any symptoms you may have. They would also discuss the recent injury affecting the feet. A podiatrist would examine the affected foot after discussing your symptoms and medical history.
A podiatrist would run various tests to look for fractures or infections such as:
Imaging Tests
- X-rays – This would provide detailed pictures of dense structures, such as bone. The X-ray would appear normal in the very early stage of Charcot. As the condition progresses to the intermediate stages, an x-ray shows fractures and dislocations of the joints.
- Magnetic resonance imaging (MRI) and ultrasound – This helps create better images of soft tissues of the foot and ankle. This is useful in diagnosing any bone infection.
- Bone scan or indium scan – A bone scan is a nuclear medicine test that helps to determine any bone infection. An indium scan is a specialized test to learn whether they are going to the bone to fight infection. Both Charcot foot and bone infection depict a positive bone scan with increased activity. But, only an infection will show increased activity on the indium scan.
TREATMENT OF CHARCOT FOOT
The goal of the treatment of Charcot arthropathy is to heal the broken bones. The treatment aim is to prevent further deformity and joint destruction. It is important to control a long-term increase in sugar level to decrease nerve damage.
Early diagnosis and treatment help in preventing further damage and avoid deformity. A podiatrist has three goals for treatment regime:
- Take the weight off the foot
- Treat the bone disease, and
- Prevent new foot fractures.
Non-Surgical Treatment – It is important to follow the podiatrist treatment plan for Charcot’s foot, especially in the case of diabetic patients. Failure to do so can lead to the loss of a toe, foot, leg, or even life.
- Immobilization – Cast is used to treat the early stages of Charcot’s foot because the foot and ankle are so fragile. During the early stage of Charcot, fragile ankle and foot must be protected so the weakened bones can repair themselves. It is important to follow complete non-weight-bearing to keep the foot from further collapsing. You should not try and put any weight on foot such as during walking until the surgeon advises. During this period, the podiatrist would recommend a fitted cast, removable boot or brace, and use crutches or a wheelchair. The healing process may take several months, although it can take considerably longer in some patients. A cast stays on the foot until the redness, swelling, and heat have subsided.
- Custom shoes and bracing – Shoes with special inserts may be needed after the bones have healed. This would enable the patient to return to daily activities and help prevent recurrence of Charcot’s foot, development of ulcers, and possibly amputation. But, braces are necessary in cases with significant deformity of the foot.
- Activity modification – Changes in activity level mane be required to avoid repetitive trauma to both feet. It is likely to develop Charcot in other feet as well, so measures must be taken to protect both feet. A podiatrist would commonly suggest using Charcot Restraint Orthotic Walker (CROW).
Surgical Treatment: Surgery is necessary if the foot deformity puts the patient at high risk for developing ulcers, or if protective shoewear is not effective. Surgery is also required for unstable fractures and dislocations to heal.
Fractures occurring in the softer bone of diabetic patients are more complex. Surgery to fix them involve plates and screws than required in people without diabetes.
Prevention of Charcot’s foot is important by controlling diabetes, regular check-ups of the foot for diabetic patients and not ignoring any swelling, redness, warm spots, or sores.
If you or anyone you know is suffering from foot problems, our expert providers at Specialty Care Clinics will take care of your health and help you recover.
Call us on (469) 545-9983 to book an appointment with our specialists.