Narcolepsy is a rare chronic neurological disorder affecting the nervous system. A nap after lunch is a habit of many people. But when the body loses its control to stay awake and people tend to sleep excessively it is categorized as Narcolepsy. The neurological disorder causes abnormal sleep affecting your quality of life.
Narcolepsy affects the ability to wake up as well as sleep and you may have the uncontrolled excessive urge to sleep anytime. You may tend to fall asleep at any time of the day or during any activity which may be very dangerous. In the sleep cycle, the body enters different stages of sleep but people suffering from narcolepsy enter the rapid eye movement stage (deep sleep stage) immediately.
Many people suffering from narcolepsy experience uneven and interrupted sleep that can involve waking up frequently during the night. You may also experience abnormal rapid eye movement (REM) sleep and can involve cataplexy, or brief attacks of muscle weakness and even lead the body to collapse.
Narcolepsy can range from mild to severe conditions, negatively impacting social activities, school, work, and overall health and well-being. A person with narcolepsy may experience fragmented sleep and excessive daytime sleepiness.
Symptoms of narcolepsy may appear in a person’s teenage years or early 20s or 30s. In the United States, approximately 50% of females in comparison to males are affected with narcolepsy. Around 1 in 2,000 people have narcolepsy as per the recent data from the experts.
TYPES OF NARCOLEPSY
Narcolepsy is categorized on basis of its severity. This includes:
- Type 1 – Narcolepsy with cataplexy. People usually are awake but experience sudden muscle weakness and lose control of the muscles in their face, arms, legs, or torso which causes slur words, have a sagging jaw, collapse, or slump over and be unable to move. This is usually caused due to the trigger of sudden strong emotion and may last for a few seconds or 2-3 minutes. Caused due to a lack of hypocretin (a chemical that regulates wakefulness as well as rapid eye movement during sleep) in the brain.
- Type 2 – Narcolepsy without cataplexy. People experience extreme sleepiness, sleep attacks, hallucinations as well as might get paralysis while falling asleep or waking up.
Secondary narcolepsy can be a result of trauma or a tumor causing damage to the hypothalamus. This is a part of the brain involved in sleep.
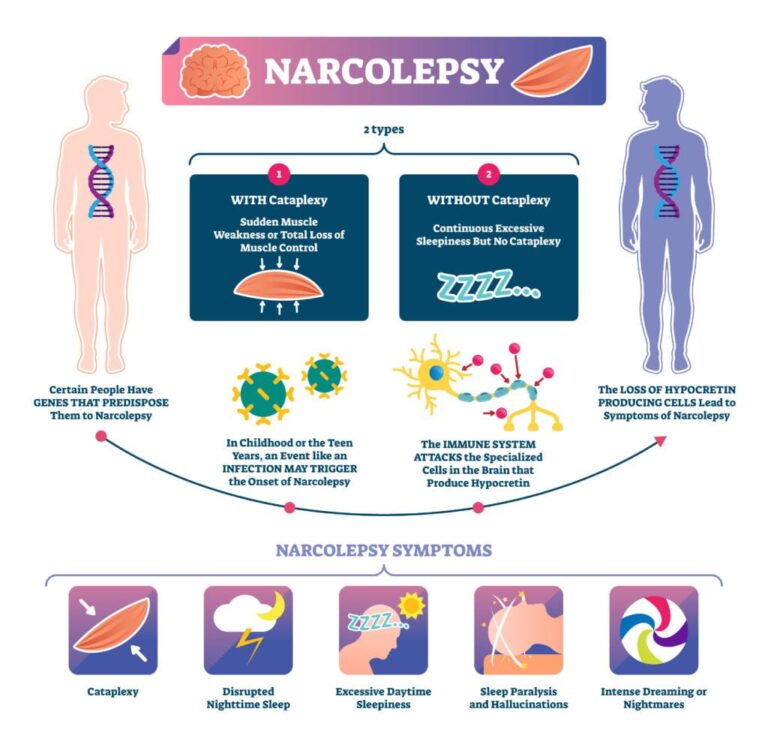
CAUSE OF NARCOLEPSY
Various reasons resulting from a combination of genetic and environmental factors lead to the development of narcolepsy. Some of these have been identified, but many remain unknown.
Narcolepsy results from the loss of a neurotransmitter or chemical signal in the brain called hypocretin or orexins. The hypocretin is essential for regulating the sleep or wake-up cycle including the rapid eye movement (REM) sleep state. When there is a shortage of hypocretin, it can lead to excessive sleepiness, and features of REM sleep, which is also called “dreaming sleep”. This may become present during wakefulness.
It has also been observed that changes in several genes, such as HLA-DQB1, influence the risk of developing narcolepsy. The genes HLA-DQB1 provide instructions for making part of a protein that plays an important role in the immune system. The variation in this gene is associated with people suffering from narcolepsy. Although, it is unclear how these genetic changes influence the risk of developing the condition.
Other possible factors that play a role in narcolepsy include:
- An autoimmune disorder: Your immune system attacks the brain cells that produce hypocretin, resulting in a shortage of this chemical.
- Family history: It can be caused when your close relatives have symptoms of narcolepsy.
- Brain injury or tumor: In a small number of patients, the area of the brain that controls REM sleep and wakefulness can be injured by trauma, tumor, or disease.
- Infections: Bacterial or viral infections such as strep throat (streptococcus), colds, and influenza may be involved in triggering narcolepsy in people who are at risk.
- Environmental toxins: Various toxins such as pesticides, heavy metals, and secondhand smoke induces narcolepsy.

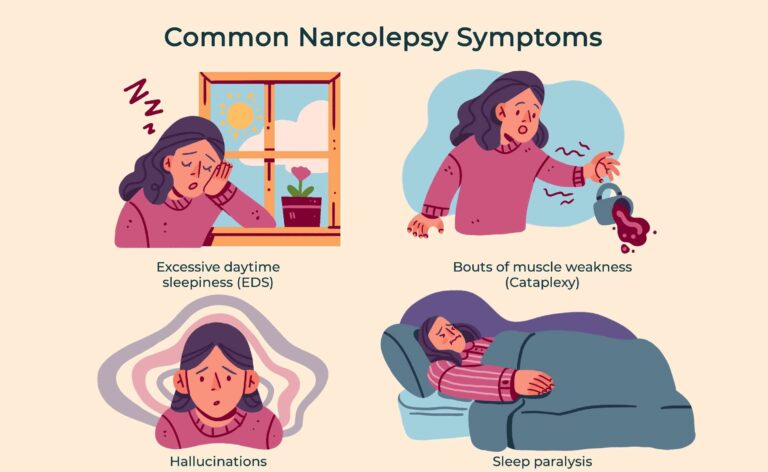
SYMPTOMS FOR NARCOLEPSY
The primary symptom of narcolepsy commonly include excessive daytime sleepiness, but it may also involve cataplexy, hypnagogic hallucinations, and sleep paralysis. The symptoms worsen during the initial years and then continue for a lifetime as there is no cure discovered yet. People may experience brain fog, poor concentration, decreased energy, memory lapses or exhaustion, and depressed mood. Some common symptoms are:
- Extreme sleepiness – You may fall asleep anytime or anywhere without any warning for an approximate half-hour. You feel refreshed after sleeping but tend to sleep again later. The focus and alertness decrease and people are not able to concentrate on their daily tasks. You may also experience mental cloudiness, a lack of energy and concentration, memory lapses, a depressed mood, and/or extreme exhaustion.
- Cataplexy – Sudden muscle tone loss which affects face, neck, and knees. This may range from mild to severe symptoms like head or jaw drop to people collapsing on the ground.
- Sleep paralysis – You may experience a temporary inability to move or speak while falling asleep or upon waking which can be frightening.
- Hallucination – If the hallucinations occur during sleep they are known as hypnagogic and if they occur while the person is awake are known as hypnopompic hallucinations. They can be vivid as well as frightening. People are confused if they are experiencing a dream or in reality.
- Disrupted night sleep – you may experience frequent awakenings during the night.
- Automatic behavior – You may fall asleep for several seconds but continue to perform routine tasks, such as eating, talking, driving, or writing, without any awareness or later memory of ever doing the task.
DIAGNOSING NARCOLEPSY
You should visit a doctor if you are experiencing the above symptoms. The doctor may run tests to help rule out other conditions that could be causing your excessive daytime sleepiness, including sleep apnoea, restless legs in bed and kicking during sleep, or an underactive thyroid gland (hypothyroidism).
The doctor may refer you to a specialist to monitor the sleep disorders who’ll analyze your sleep patterns. The specialist would confirm the disorder with the polysomnogram (PSG) and the multiple sleep latency tests (MSLT).
TREATING NARCOLEPSY
Treatment and management of narcolepsy consist of medications and lifestyle changes. Medications aim to reduce daytime sleepiness and improve alertness.

-
- Medication: Various medications such as wake-promoting medications, sodium oxybate, and antidepressants help in controlling narcolepsy.
- Lifestyle changes: certain changes in lifestyle help manage narcolepsy, which include:
- Regular Sleep
- Avoid alcohol and caffeine
- Avoid smoking
- Exercise
- Take short naps Avoid large, heavy meals right before bedtime

OUTLOOK
Narcolepsy is a life-long sleeping disorder. But, it usually does not worsen with age. The use of medications and lifestyle changes can help improve narcolepsy symptoms. Narcolepsy impacts your ability to drive. With correct diagnosis, working with your doctor to find the best treatment for you, and following the above tips, you can continue living a healthy life.
If you or anyone you know is suffering from neurological disorders, our expert providers at Specialty Care Clinics will take care of your health and help you recover.
Call 469-545-9983 to book a telehealth appointment for an at-home check-up.
