WET MACULAR DEGENERATION – SYMPTOMS, CAUSES, AND TREATMENT
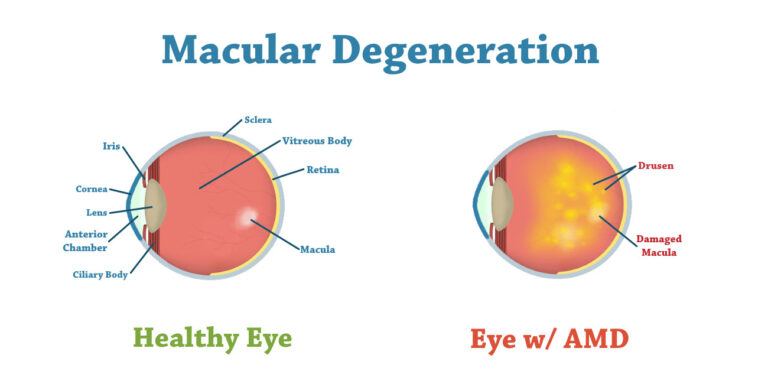
Wet macular degeneration is a chronic eye disorder that causes blurred vision or a blind spot in your field of vision. It is usually caused by abnormal blood vessels that leak fluid or blood into the macula. The macula is in the part of the retina accountable for the central vision.
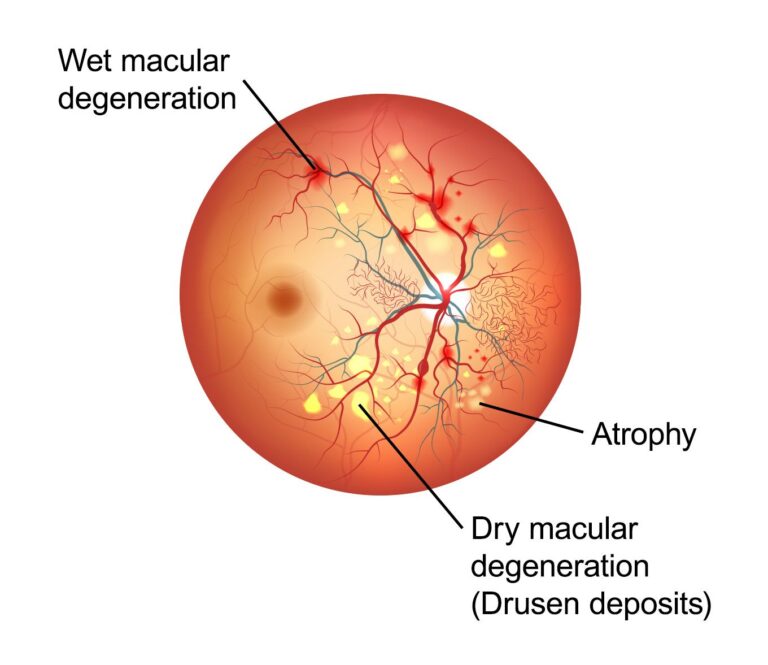
Wet macular degeneration is one of two types of age-associated macular degeneration. The other type — dry macular degeneration — is more common and less serious. The wet type always starts out as the dry type.
Early detection and treatment of wet macular degeneration might help reduce vision loss and, in some instances, recover vision.
SYMPTOMS
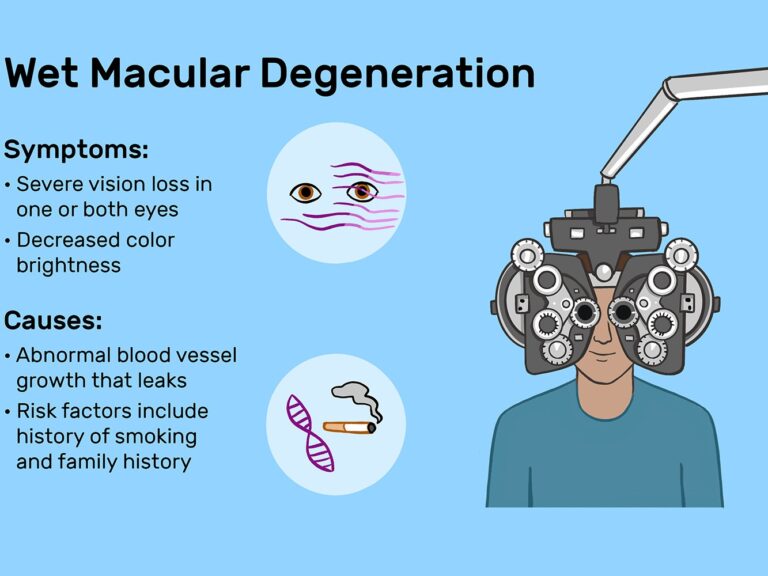
Wet macular degeneration symptoms generally appear suddenly and worsen rapidly. They might include:
- Visual distortions, like straight lines seeming bent
- Decreased central vision in one or both eyes
- The requirement for brighter light when reading or doing close-up work
- Increased difficulty adapting to low light levels, like when entering a dimly lit restaurant
- Increased blurriness of printed words
- Decreased intensity or brightness of colors
- Trouble recognizing faces
- A well-defined blurry spot or a blind spot in your visual field
Macular degeneration does not affect side (peripheral) vision, so it rarely causes total blindness.
WHEN SHOULD YOU SEE A DOCTOR?
See your eye doctor if:
- You notice changes in your central vision
- Your ability to see colors and fine detail becomes damaged
These changes might be the first indication of macular degeneration, particularly if you are older than age 60.
CAUSES
No one knows the accurate cause of wet macular degeneration, but it develops in people who have had dry macular degeneration. Of all people with age-associated macular degeneration, about twenty percent have the wet form.
Wet macular degeneration could develop in different ways:
- Vision loss caused by abnormal blood vessel growth – At times abnormal new blood vessels grow from the choroid under and into the macula (choroidal neovascularization). The choroid is the layer of blood vessels in between the retina and the outer, firm coat of the eye (sclera). These abnormal blood vessels might leak fluid or blood, interfering with the retina’s function.
- Vision loss caused by fluid build-up in the back of the eye – When fluid leaks from the choroid, it could collect between the thin cell layer known as the retinal pigment epithelium and the retina or within the layers of the retina. This might cause a bump in the macula, resulting in vision loss or distortion.
RISK FACTORS
Factors that might increase your risk of macular degeneration include:
- Age – This disease is most common in people over the age of 55.
- Family history and genetics – This disease has an inherited component. Researchers have identified several genes associated with developing the condition.
- Race – Macular degeneration is more common among Caucasians.
- Smoking – Smoking cigarettes or being frequently exposed to smoke significantly increases your risk of macular degeneration.
- Obesity – Research suggests that being obese increases the chance that early or intermediate macular degeneration will progress to a more severe form of the disease.
- Cardiovascular disease – If you have diseases that affect your heart and blood vessels, you might be at higher risk of macular degeneration.
COMPLICATIONS
People whose wet macular degeneration has progressed to central vision loss have a greater risk of depression and social isolation. With the profound loss of vision, people might see visual hallucinations (Charles Bonnet syndrome).
PREVENTION
It is important to have routine eye examinations to identify early signs of macular degeneration. The following measures might help reduce your risk of developing wet macular degeneration:
- Manage your other medical conditions – For instance, if you have cardiovascular disease or high blood pressure, take your medication and follow your doctor’s instructions for controlling the condition.
- Do not smoke – Smokers are at a higher risk of developing macular degeneration than are non-smokers. Ask your doctor for help to quit smoking.
- Maintain a healthy weight and exercise regularly – If you need to lose weight, decrease the number of calories you eat and increase the amount of exercise you get each day.
- Choose a diet rich in fruits and vegetables – Choose a healthy diet that is full of a variety of fruits and vegetables. These foods contain antioxidant vitamins that lower your risk of developing macular degeneration.
- Include fish in your diet – Omega-3 fatty acids, which are found in fish, might reduce the risk of macular degeneration. Nuts, like walnuts, also consist of omega-3 fatty acids.
DIAGNOSIS
Your doctor will review your medical and family history and conduct a complete eye examination. To confirm a diagnosis of macular degeneration, he or she might do several other tests, including:
- Examination of the back of your eye – Your eye doctor will put drops in your eyes to dilate them and use a special instrument to check the back of your eye. He or she will look for fluid or blood or a mottled appearance that is caused by drusen. People with macular degeneration usually have many drusen—yellow deposits that form under the retina.
- Test for defects in the center of your vision – During an eye examination, your eye doctor might use an Amsler grid to test for defects in your central vision. If you suffer from macular degeneration, some of the straight lines in the grid will look faded, broken, or distorted.
- Fluorescein angiography – During this test, your doctor administers a colored dye into a vein in your arm. The dye travels to and indicates the blood vessels in your eye. A special camera takes images as the dye travels through the blood vessels. The pictures will show if you have leaking abnormal blood vessels or retinal changes.
- Indocyanine green angiography – Similar to fluorescein angiography, this test uses an injected dye. It might be used to confirm the findings of a fluorescein angiography or to identify abnormal blood vessels deeper in the retina.
- Optical coherence tomography – This non-invasive imaging test shows detailed cross-sections of the retina. It highlights areas of thinning, thickening, or swelling. This test is also used to help track how the retina responds to macular degeneration treatments.
- Optical coherence tomography (OCT) angiography – This is a newer, non-invasive test that, in specific cases, enables your doctor to visualize unwanted blood vessels in the macula. Though still used mainly as a research tool, it is gaining in popularity in clinics.

TREATMENT
Treatments are available that might help slow disease progression, preserve existing vision and if started early enough, recover some lost vision.
Medications
Medications might help stop the growth of new blood vessels by blocking the effects of growth signals the body sends to generate new blood vessels. These medications are considered the first-line treatment for all stages of wet macular degeneration.
Medications used to treat wet macular degeneration are:
- Bevacizumab (Avastin)
- Ranibizumab (Lucentis)
- Aflibercept (Eylea)
- Brolucizumab (Beovu)
Your doctor administers these medications to the affected eye. You might require injections every four to six weeks to maintain the beneficial effect of the medication. In some instances, you might partially recover vision as the blood vessels shrink and the fluid under the retina absorbs, allowing some vision gain.
Possible risks of eye injections are conjunctival hemorrhage, increased eye pressure, infection, retinal detachment, and eye inflammation.
Therapies
- Photodynamic therapy – This procedure is very often used to treat abnormal blood vessels at the center of your macula. During photodynamic therapy, your doctor administers a drug known as verteporfin (Visudyne) into a vein in your arm, which travels to blood vessels in your eye. Your doctor shines with a focused light from a special laser to the abnormal blood vessels in your eye. This activates the drug, causing the abnormal blood vessels to close, thereby stopping the leakage.
Photodynamic therapy might improve your vision and reduce the rate of vision loss. You might need repeated treatments over time, as the treated blood vessels might reopen. After photodynamic therapy, you will need to avoid direct sunlight and bright lights until the drug has cleared your body, which might take a few days. - Photocoagulation – During photocoagulation therapy, your doctor uses a high-energy laser beam to seal the abnormal blood vessels below the macula. The laser causes scarring that could create a blind spot, but the procedure is used to stop the vessels from bleeding with the goal of minimizing further damage to the macula. Even with this treatment, blood vessels might regrow, requiring further treatment.
Few people suffering from wet macular degeneration are candidates for this treatment. It usually is not an option if you have abnormal blood vessels directly under the center of the macula. Also, the more damaged your macula is, the lower the probability of success. - Low vision rehabilitation – Age-associated macular degeneration does not affect your side (peripheral) vision and generally does not cause total blindness. But it could reduce or eliminate your central vision — which is necessary for driving, reading, and recognizing people’s faces. It might be beneficial for you to work with a low vision rehabilitation specialist, an occupational therapist, your eye doctor, and others trained in low vision rehabilitation. They could help you find ways to adapt to your changing vision.
If you or anyone you know is suffering from wet macular degeneration, our expert providers at Specialty Care Clinics will take care of your health and help you recover.
Call us on (469) 545-9983 to book an appointment with our specialists.
