WHAT IS MYOFASCIAL PAIN SYNDROME?
Myofascial pain syndrome is a painful condition that affects your muscles and fascia. “Myo” stands for muscle and “fascial” stands for fascia. Your fascia is the thin, white connective tissue that is wrapped up around every muscle.
If your body was orange, your skin would be the outside orange peel, your muscles would be the fleshy orange fruit itself and the thin white membrane encircling each orange segment would be the fascia. Fascia encircles every level of muscle tissue muscle fibers, single muscles, and muscle groups.
Muscle pain is not picky it could strike anyone at any time in their life. Everyone from the mother carrying her child and the roofer laying shingles to the best friend helping lift boxes during a move could experience muscle pain. Unfortunately, for some people, this pain could be unbearable and it sticks around long after it should have faded. If you have muscle pain that does not go away for a long period of time, it can be myofascial pain.
WHAT DOES THE FASCIA DO?
Simply put, your fascia holds your muscles together, which permits them to contract and stretch. Fascia also offers a slick surface so that individual muscle fibers, single muscles, and muscle groups could slide against each other without creating friction, tearing, or causing other issues.
In fact, fascia is everywhere inside your body. Besides your muscles, all organs and blood vessels are joined to or encircled by fascia. Fascia is a complicated substance. It consists of nerve endings. Scientists continue to discover all the features and roles of the fascia.
WHAT HAPPENS WHEN A PERSON SUFFERS FROM MYOFASCIAL PAIN SYNDROME? HOW DOES IT BEGIN?
Myofascial pain syndrome is a commonly occurring condition. If you suffer from myofascial pain syndrome, you might feel pain and tenderness in muscles in a specific region of your body. This pain and tenderness are usually associated with one or more “trigger points.” To the touch, trigger points look like small bumps, nodules, or knots in your muscle.
If you could look at a trigger point under a microscope, you would see that it lies within a taut band, which is a tight strand of muscle that looks like a cord or tendon. The trigger point itself the “knot” is actually many nearby segments of muscle fibers that are stuck in the contracted condition.
When the muscle fibers are stuck in contraction, blood flow stops. If blood flow to the region stops, that region of muscle is not getting the oxygen it requires. Waste materials also accumulate in these fibers. This irritates the trigger point, which responds by sending out a pain signal. Your brain reacts by telling you not to use that muscle.
Lack of use actually causes the muscle to tighten, become weak and it causes a loss in your extent of motion. Muscles around the damaged muscle have to work harder to do the work of the damaged muscle. Trigger points could develop in these muscles too and add to the localized pain you feel.
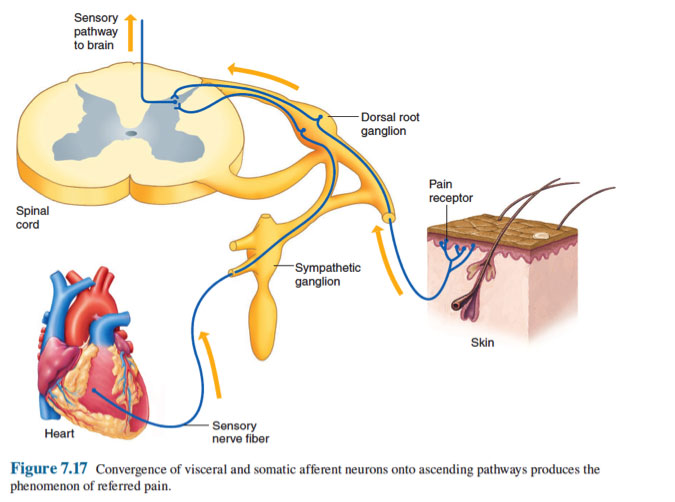
Trigger points could develop in all muscles, and in many muscles at the same time. This is one of the reasons why it might seem like your pain in shifting or moving around. Trigger points could also be tricky in that pain could happen at the area of the trigger point (when lightly pressed) or cause pain in a nearby region. This is known as referred pain.
HOW COMMON IS MYOFASCIAL PAIN SYNDROME?
Myofascial pain happens in about 85 percent of people sometime during their life. Even this high percentage might not be accurate. Myofascial pain is usually underdiagnosed, misdiagnosed, or overlooked because it is hidden in other types of diagnosis like headache, neck and shoulder pain, pelvic pain, limb pain, or nerve pain syndrome.
Men and women are equally damaged, though middle-aged inactive women are at the highest risk.
WHERE DOES MYOFASCIAL PAIN SYNDROME MOST COMMONLY HAPPEN?
Myofascial pain and trigger points could develop in any muscle in the body. Although, the most commonly damaged muscles are those in the upper back, shoulder, and neck. These muscles include the:
- Sternocleidomastoid – This big muscle helps rotate your head to the opposite side and flexes your neck. It is situated on both sides of your neck, running from your skull behind your ear region to your collarbone and breast bone.
- Trapezius – This big, broad, flat triangular back muscle tilts and turns your head and neck, shrugs and steadies your shoulders, and twists your arms. The muscle extends from the bottom of your skull to the middle of your back.
- Levator scapulae – This pair of strap-like muscles help lift and rotate each of your shoulder blades. They run from the first 4 cervical vertebrae to the top edge of your shoulder.
- Infraspinatus – This triangular muscle, situated on the backside of each of your shoulder blades, helps rotate and stabilize your shoulder joints. It is 1 of 4 muscles of the rotator cuff.
- Rhomboids – This pair of upper back muscles pull your shoulder blades together when they contract and fasten the upper limbs to your shoulder blade. These muscles run diagonally from the neck and chest vertebrae of the spine down to the rear of the shoulder blades.

MYOFASCIAL PAIN SYNDROME SYMPTOMS
Symptoms are different for each individual with myofascial pain syndrome. Sometimes the pain occurs unexpectedly and all at once, and that is known as a “flare-up” of symptoms. At other times it is a constant, dull pain that sort of lingers in the background.
Symptoms of myofascial pain syndrome include:
- Pain is described as deep aching, throbbing, tight, stiff, or vice-like.
- Trigger points (a small bump, nodule, or knot in the muscle that causes pain when touched and sometimes when it is not touched).
- Muscles that are tender or sore.
- Weakness in the affected muscle(s).
- Reduced range of motion in the affected regions (for example, you might be unable to completely rotate your shoulder).
People with myofascial pain syndrome usually have other health problems that coincide. Commonly reported problems to include:
- Headaches
- Poor sleep
- Stress, anxiety, depression
- Feeling tired (fatigue)
- Muscle strain and pain
MYOFASCIAL PAIN SYNDROME CAUSES
The jury is still out about all of the causes, contributing factors, and precisely how the pain mechanism works.
Causes of myofascial pain syndrome include:
- Muscle injury
- Muscle strain/repetitive muscle use (for example hammering)
- Muscle weakness/lack of muscle activity (for example a leg in a cast will not get enough movement).
- Poor posture.
- Working in or living in a cold climate.
- Emotional stress (could cause muscle tension)
- Pinched nerve.
Other factors which may contribute to the development of myofascial pain syndrome include:
- Metabolic or hormonal problems like thyroid disease or diabetic neuropathy
- Vitamin deficiencies, including vitamin D and folate
- Presence of chronic infections
IS MYOFASCIAL PAIN SYNDROME AN AUTOIMMUNE DISEASE?
It’s not. Swelling of the muscle or fascia is not caused by your body’s immune system incorrectly attacking healthy cells. Instances of autoimmune diseases are lupus, type 1 diabetes, celiac disease, and multiple sclerosis.

MYOFASCIAL PAIN SYNDROME PREVENTION
There are specific factors that could put you more at risk for developing myofascial pain syndrome. Managing these risk factors might not prevent you from developing the syndrome, but could help reduce the severity of the condition.
Several prevention suggestions to follow are also pain management strategies:
- Maintain proper sleep hygiene
- Reduce your stress
- Get exercise
- Avoid preventable muscle injury. (For example, is the shoulder bag/purse you carry too heavy and digging into the muscles in your shoulder?)
- Practice relaxation methods
- Eat a healthy diet, like the Mediterranean diet
- Myofascial pain syndrome
Some foods cause swelling, and swelling increases myofascial pain. Some foods to avoid include:
- Fried foods (French fries, for instance).
- Dairy (milk, cheese, yogurt).
- Refined carbohydrates and foods with refined flour (pastries, white bread, pastas, breakfast cereals, and pizza).
- Margarine (butter), vegetable oil.
- Sugary foods and beverages like soft drinks.
- Red meat (burgers, steaks).
- Artificial sweeteners and general additives (“no sugar added” products, zero-calorie “diet” soft drinks, processed foods that include fruit, ice cream, and candy).
- Processed meat (hot dogs, sausage).
Check your cupboards and your fridge. Empty it of any foods that will raise your myofascial pain syndrome symptoms.
MYOFASCIAL PAIN SYNDROME DIAGNOSIS
Myofascial pain syndrome is usually an underdiagnosed and overlooked condition. It may be mistaken for a problem with your nerves, bones, ligaments, or tendons — but it is not. That is the problem with your muscles.
There are no tests no imaging tests, lab tests/ blood tests, electromyography, or muscle biopsy that could diagnose myofascial pain syndrome. In addition to this, there are no visible signs, like redness, inflammation, or unusual muscle warmth.
The best method your healthcare provider could use to detect this syndrome is to physically examine your muscles to feel for the taut bands of muscles and then find the precise spots of tenderness. Finding and applying pressure at a trigger point will cause pain, felt at the immediate point or in a region at a short distance away (referred pain).
There are 4 types of trigger points:
- An active trigger point is generally found in a muscle and pressure to it results in local or regional pain.
- A latent trigger point has the potential to be active, however, it is dormant.
- A secondary trigger point is situated within a muscle other than the one that holds the active trigger point. It could be irritated at the same time as the active trigger point.
- A satellite trigger point is one that becomes inactive because it overlaps with the area of other trigger points.
Referred Pain
WHAT IS THE DIFFERENCE BETWEEN MYOFASCIAL PAIN SYNDROME AND FIBROMYALGIA?
Myofascial pain and fibromyalgia pain feel the same. Both have trigger points that radiate pain. Although, while myofascial pain is contained in one certain area (or, if more than one area, those areas are generally on the same side of the body), fibromyalgia pain is felt throughout the entire body. A patient with fibromyalgia has more trigger points, general pain, worse fatigue and sleep problems, headaches, an irritable bowel, a sensation of inflammation, and sometimes burning, prickling, or tingling feeling. Some researchers believe that myofascial pain syndrome could transition into fibromyalgia.

MYOFASCIAL PAIN SYNDROME TREATMENT
If you suffer from myofascial pain syndrome, treatment will be more successful if you see your healthcare provider soon after symptoms develop before trigger points are established. Many treatments are available and your medical professional will likely use a combination of the following to manage your pain and restore damaged muscles:
- Physical therapy or physiotherapy (to strengthen, stretch, and relax muscles).
- Dry needling (pushing thin needles into the trigger point to lower tightness, increase blood circulation, and ease the pain).
- Wet needling/trigger point injections (use of a needle to inject or administer lidocaine [or another anesthetic] into the trigger point to ease the pain).
- “Spray and stretch” (spraying a trigger point with a coolant, then gradually, manually stretching the muscles).
- Low-level light therapy / cold laser (use of lasers to stimulate the release of pain-relieving chemicals).
- Ultrasound (using sound waves to penetrate muscles).
- Transcutaneous electrical nerve stimulation (TENS therapy pads are connected to your skin through which low-voltage electrical signals are sent).
- Acupuncture and relaxation therapies, including biofeedback and cognitive behavioral therapy (also good for improving sleep and lowering anxiety).
Prescription medication options might include:
- Pain-killing medications (analgesics)
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Muscle relaxants
- Steroids
- Antidepressants
- Some sedatives to improve the quality of your sleep
Treatments you could do at home include:
- Heat (as in a heating pad). Some individuals benefit from cold/ice packs
- Exercise. Particularly weight-bearing exercises (to strengthen muscles), stretching exercises (to stretch muscles), and aerobic exercises (to get more oxygen into the muscles)
- Over-the-counter pain killers (like acetaminophen) or NSAIDs (like ibuprofen or naproxen). Do not take these drugs if you are taking analgesics or NSAIDs prescribed by your healthcare provider
- Relaxation techniques, including yoga (to stretch and relax muscles and reduce stress), breathing exercises, and meditation
- Dietary changes (avoid foods known to cause swelling)
- Soaking in warm water
- Massages
The duration of myofascial pain syndrome differs from person to person. With treatment, it might go away after a day or a few weeks, but it could take longer for some. How fast your myofascial pain syndrome resolves depends on several factors, including:
- Your general health
- Diet
- Amount and quality of sleep
- How carefully you obey your healthcare provider’s recommendations

WHO WILL TREAT/MANAGE MY MYOFASCIAL PAIN SYNDROME?
Healthcare providers generally capable of managing myofascial pain syndrome include physiatrists (medical doctors who specialize in physical medicine and rehabilitation), pain management specialists, rheumatologists or orthopedists, and physical therapists.
MYOFASCIAL PAIN SYNDROME PROGNOSIS
Each individual’s pain location of pain and severity is unique. Pain could flare up from time to time or be ongoing and long-lasting. Successful treatment generally needs finding healthcare providers you are comfortable with and following their treatment and management plan for lowering your pain.
If you or anyone you know is suffering from myofascial pain syndrome, our expert providers at Specialty Care Clinics will take care of your health and help you recover.
Call 469-805-4561 to book an telehealth appointment for an at-home check-up.
