WHAT IS VULVODYNIA?
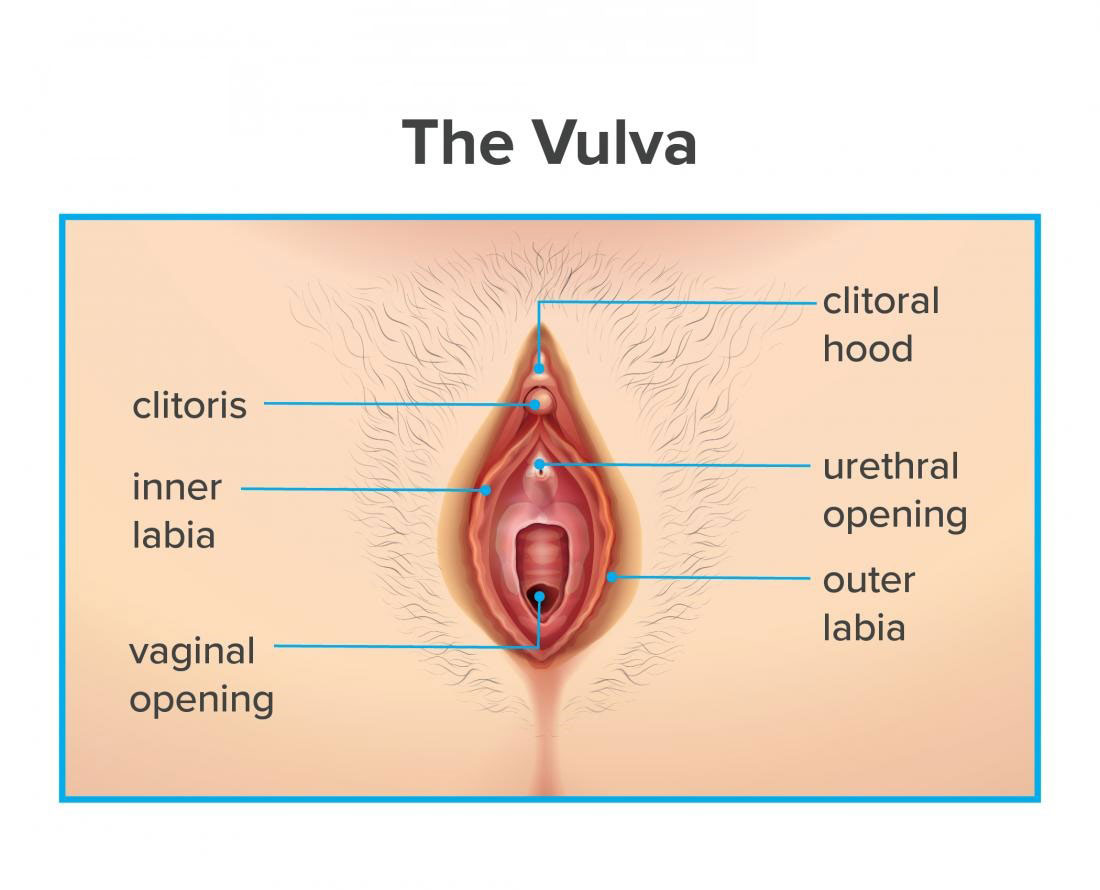
Vulvodynia is chronic pain or discomfort around the opening of your vagina (vulva) for which there is no identifiable cause and which lasts at least 3 months. The pain, burning, or irritation related to vulvodynia could make you so uncomfortable that sitting for long periods or having sex becomes unthinkable. The condition could last for months to years.
If you have vulvodynia, do not let the absence of visible signs of embarrassment about discussing the symptoms keep you from seeking help. Treatment options are available to lower your discomfort. And your doctor may be able to determine a cause for your vulvar pain, so it is important to have an examination.
SYMPTOMS
The main vulvodynia symptom is pain in your genital region, which could be characterized as:
- Burning
- Soreness
- Stinging
- Rawness
- Painful intercourse (dyspareunia)
- Throbbing
- Itching

Your pain may be constant or occasional. It may happen only when the sensitive area is touched (provoked). You may feel the pain in your whole vulvar area (generalized), or the pain may be localized to a certain area, like the opening of your vagina (vestibule).
Vulvar tissue may look slightly inflamed or swollen. More usually, your vulva appears normal.
An identical condition, vestibulodynia, causes pain only when pressure is applied to the region surrounding the entrance to your vagina.
WHEN SHOULD YOU SEE A DOCTOR?
However, women usually do not mention vulvodynia to their doctors, the condition is fairly common.
If you have pain in your genital area, talk about it with your doctor or ask for a referral to a gynecologist. It is crucial to have your doctor rule out more easily treatable causes of vulvar pain — for example, yeast or bacterial infections, herpes, precancerous skin conditions, genitourinary syndrome of menopause, and medical problems like diabetes.
It is also important not to repeatedly use over-the-counter treatments for yeast infections without seeing your doctor. Once your doctor has evaluated your symptoms, he or she could recommend treatments or ways to help you manage your pain.
CAUSES
Doctors do not know what causes vulvodynia, but possible contributing factors include:
- Injury to or irritation of the nerves surrounding your vulvar area
- Past vaginal infections
- Allergies or sensitive skin
- Hormonal changes
- Muscle spasm or weakness in the pelvic floor, that supports the uterus, bladder, and bowel

COMPLICATIONS
Because it could be painful and frustrating and could keep you from wanting sex, vulvodynia could cause emotional issues. For instance, fear of having sex could cause spasms in the muscles around your vagina (vaginismus). Other complications may include:
- Anxiety
- Depression
- Sleep disturbances
- Sexual dysfunction
- Altered body image
- Relationship problems
- Decreased quality of life
DIAGNOSIS
Before diagnosing vulvodynia, your doctor will ask you questions about your medical, sexual and surgical history and determine the location, nature, and extent of your symptoms.
Your doctor may also perform a:
- Pelvic examination – Your doctor visually checks your external genitals and vagina for signs of infection or other causes of your symptoms. Even if there is no visual evidence of infection, your doctor may take a sample of cells from your vagina to test for an infection, like a yeast infection or bacterial vaginosis.
- Cotton swab test – Your doctor uses a moistened cotton swab to gently check for specific, localized areas of pain in your vulvar area.

TREATMENT
Vulvodynia treatments concentrate on relieving symptoms. No one treatment works in each case. For many, a combination of treatments works better. It could take time to find out the correct treatments, and it could take time after starting treatment before you notice relief.
Treatment options are as follows:
- Medications – Steroids, tricyclic antidepressants, or anticonvulsants could help lower chronic pain. Antihistamines may lower itching.
- Biofeedback therapy – This therapy could help lower pain by teaching you how to relax your pelvic muscles and control how your body responds to the symptoms.
- Local anesthetics – Medications, like lidocaine ointment, could provide temporary symptom relief. Your doctor may recommend applying lidocaine thirty minutes before sexual intercourse to lower your discomfort. Using lidocaine ointment could cause your partner to have momentary numbness after sexual contact.
- Nerve blocks – Women who have long-standing pain that does not respond to other treatments may benefit from local nerve block injections.
- Pelvic floor therapy – Many women with vulvodynia have tension in the muscles of the pelvic floor, that support the uterus, bladder, and bowel. Exercises to relax those muscles could help relieve vulvodynia pain.
- Surgery – In cases of localized vulvodynia or vestibulodynia, surgery to remove the damaged skin and tissue (vestibulectomy) eases pain in some women.
If you or anyone you know is suffering from vulvodynia, our expert providers at Specialty Care Clinics will take care of your health and help you recover.
Call us on (469) 545-9983 to book an appointment with our specialists.
