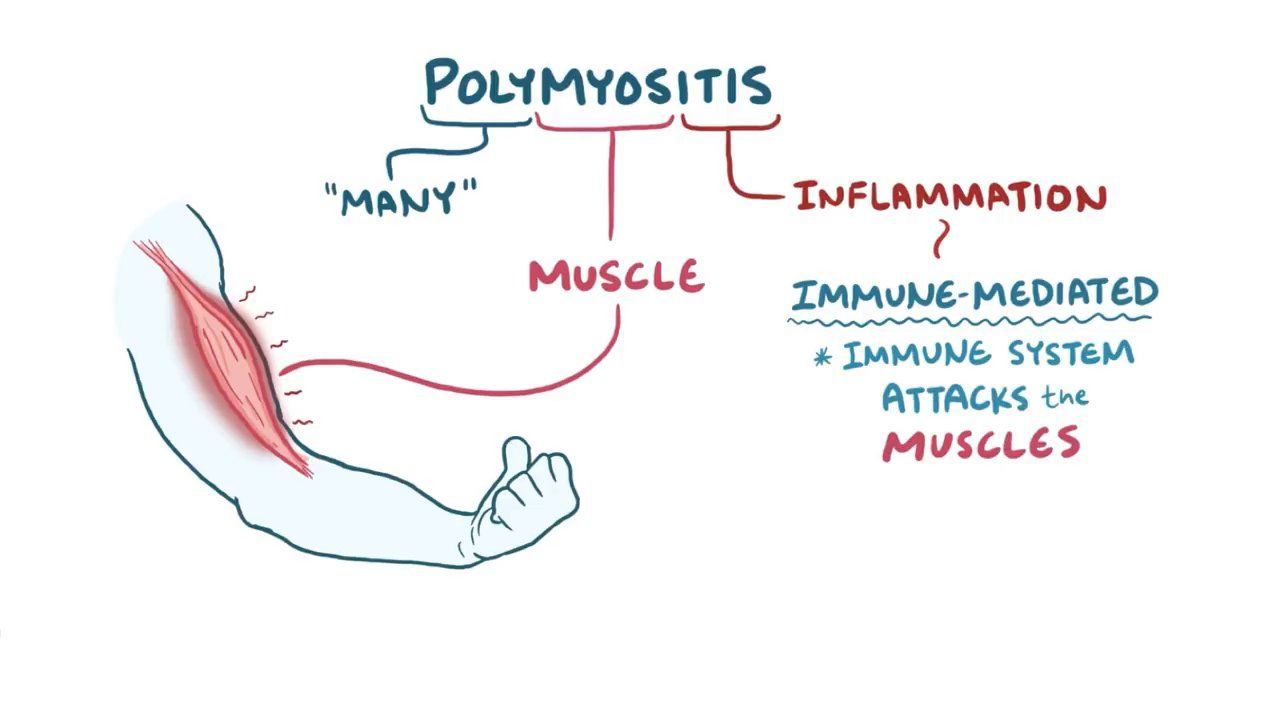
WHAT IS POLYMYOSITIS?
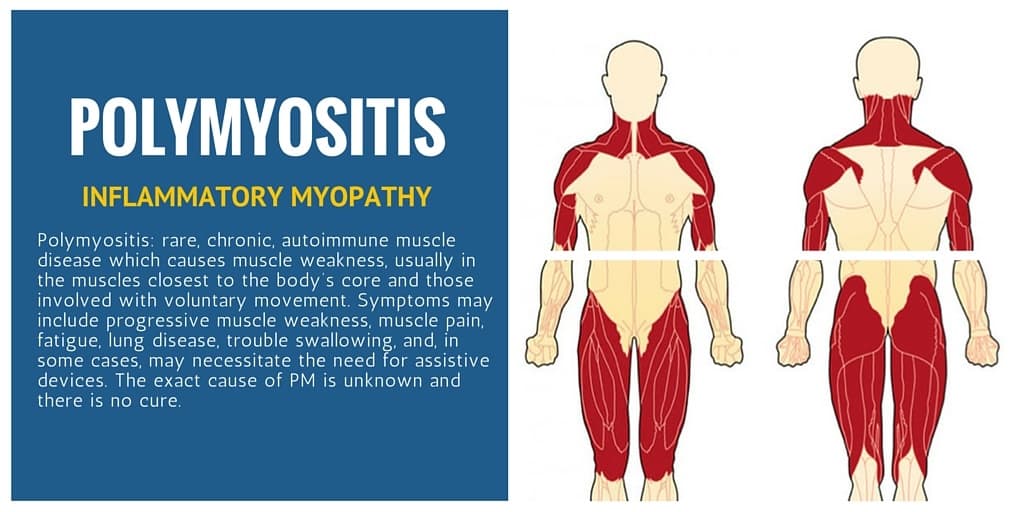
Polymyositis is also known as inflammatory myopathy is an unusual inflammatory disease that causes muscle weakness affecting both sides of your body. Having this condition could make it difficult to climb stairs, rise from a seated position, lift objects or reach overhead.
Polymyositis most frequently affects adults in their 30s, 40s, or 50s. It is more common in blacks than in whites, and women are affected more usually than men. Signs and symptoms usually develop slowly, over weeks or months.
While there is no cure for polymyositis, treatment — ranging from medications to physical therapy — could improve your muscle strength and function.
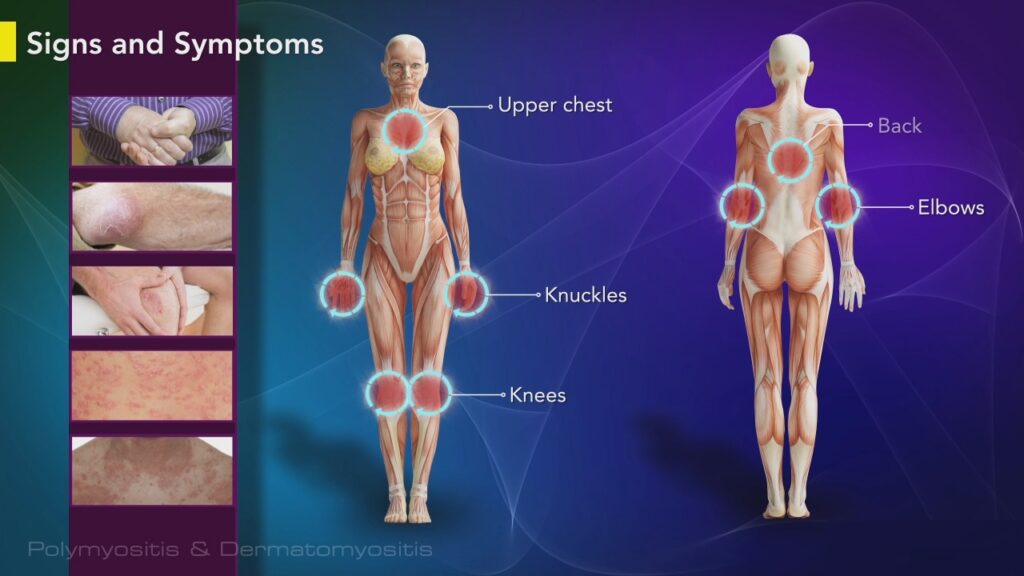
POLYMYOSITIS SYMPTOMS
The muscle weakness related to polymyositis involves the muscles closest to the trunk, like those in your hips, thighs, shoulders, upper arms, and neck. The weakness affects both the left and right sides of your body and tends to slowly get worse.
WHEN SHOULD YOU SEE A DOCTOR?
Look for medical attention if you develop unexplained muscle weakness.
POLYMYOSITIS CAUSES
The exact cause of polymyositis is not known, but the disease shares many characteristics with autoimmune disorders, in which your immune system mistakenly attacks your own body tissues.
POLYMYOSITIS RISK FACTORS
Your risk of polymyositis is greater if you have lupus, rheumatoid arthritis, scleroderma, or Sjogren’s syndrome.
POLYMYOSITIS COMPLICATIONS
Potential complications of polymyositis include:
- Difficulty swallowing – If the muscles in your esophagus are affected, you might have problems swallowing (dysphagia), which in turn might cause weight loss and malnutrition.
- Aspiration pneumonia – Difficulty swallowing might also cause you to breathe food or liquids, including saliva, into your lungs (aspiration), which could lead to pneumonia.
- Breathing problems – If your chest muscles are affected by the disease, you might experience breathing problems, like shortness of breath or, in severe cases, respiratory failure.
Associated conditions
However, these are not complications, polymyositis is usually related to other conditions that might cause further complications of their own, or in combination with polymyositis symptoms. Related conditions include:
- Raynaud’s phenomenon – This is a condition where your fingers, toes, cheeks, nose, and ears initially turn pale when exposed to cold temperatures.
- Other connective tissue diseases – Other conditions, like lupus, rheumatoid arthritis, scleroderma, and Sjogren’s syndrome, could happen in combination with polymyositis.
- Cardiovascular disease – Polymyositis might cause the muscular walls of your heart to become swollen (myocarditis). In a small number of people with polymyositis, congestive heart failure and heart arrhythmias might develop.
- Lung disease – A condition known as interstitial lung disease might happen with polymyositis. Interstitial lung disease means a group of disorders that cause scarring (fibrosis) of lung tissue, making lungs stiff and inelastic. Signs and symptoms involve a dry cough and shortness of breath.
- Cancer – People who have polymyositis have an increased risk of cancer.
POLYMYOSITIS DIAGNOSIS
If your doctor suspects that you have polymyositis, he or she may recommend some of the following tests:
- Blood tests – A blood test will let your doctor know if you have increased levels of muscle enzymes, which could indicate muscle damage. A blood test could also detect specific autoantibodies related to different symptoms of polymyositis, which could help in determining the best medication and treatment.
- Electromyography – This test includes inserting a slim needle electrode through the skin into the muscle. Electrical activity is measured as you relax or tighten the muscle, and changes in the pattern of electrical activity could confirm a muscle disease. The doctor could determine the distribution of the disease by testing different muscles.
- Magnetic resonance imaging (MRI) – A scanner creates cross-sectional pictures of your muscles from data generated by a powerful magnetic field and radio waves. Unlike a muscle biopsy, an MRI could assess inflammation over a large area of muscle.
- Muscle biopsy – During this test, a tiny piece of muscle tissue is surgically removed for lab analysis. Analysis might reveal abnormalities, like inflammation, damage, certain proteins, or enzyme deficiencies.

POLYMYOSITIS TREATMENT
Although there is no cure for polymyositis, treatment could improve your muscle strength and function. The previous treatment is started in the course of polymyositis, the more effective it is — leading to fewer complications.
However, as with many conditions, no single approach is best; your doctor will customize your treatment strategy based on your symptoms and how well they respond to therapy.
POLYMYOSITIS MEDICATIONS
The most frequently used medications to treat polymyositis include:
- Corticosteroids – Medications like prednisone could be very effective in controlling polymyositis symptoms. But prolonged use of these medications could have severe and wide-ranging side effects, which is why your doctor might slowly taper the dose of medication down to lower levels.
- Corticosteroid-sparing agents – When used in combination with a corticosteroid, these medications could decrease the dose and possible side effects of the corticosteroid. The two most frequent medications used for polymyositis are azathioprine (Azasan, Imuran) and methotrexate (Trexall). Other medications recommended for polymyositis involve mycophenolate mofetil (CellCept), cyclosporine, and tacrolimus.
- Rituximab (Rituxan) – More commonly used to treat rheumatoid arthritis, rituximab is an option if initial therapies do not adequately control your polymyositis symptoms.
Therapy
Depending on the severity of your symptoms, your doctor may recommend:
- Physical therapy – A physical therapist could show you exercises to maintain and improve your strength and flexibility and advise an appropriate level of activity.
- Speech therapy – If your swallowing muscles are weakened by polymyositis, speech therapy could help you learn how to compensate for those changes.
- Dietetic assessment – Later in the course of polymyositis, chewing and swallowing could become more difficult. A registered dietitian could teach you how to prepare easy-to-eat, nutritious foods.
Surgical and other procedures
Intravenous immunoglobulin (IVIg) is a purified blood product that consists of healthy antibodies from thousands of blood donors. These healthy antibodies could block the damaging antibodies that attack muscle in polymyositis. Given as an infusion through a vein, IVIg treatments might need to be repeated regularly for the effects to continue.
If you or anyone you know is suffering from polymyositis, our expert providers at Specialty Care Clinics will take care of your health and help you recover.
Call (469) 545-9983 to book a telehealth appointment for an at-home check-up.
