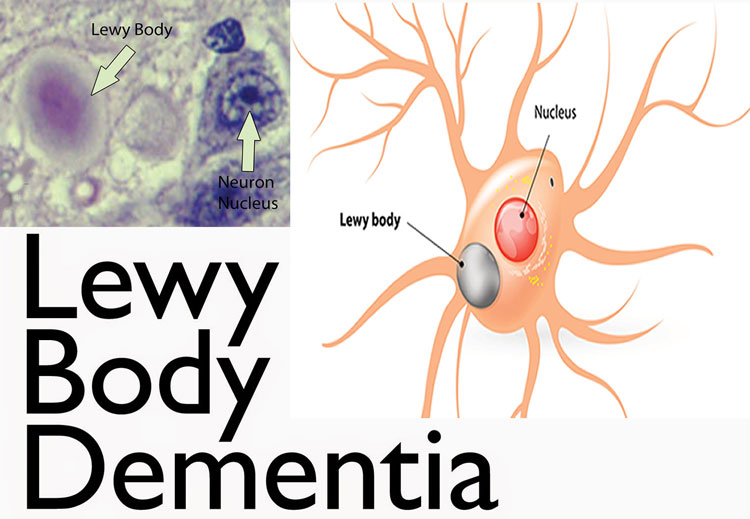
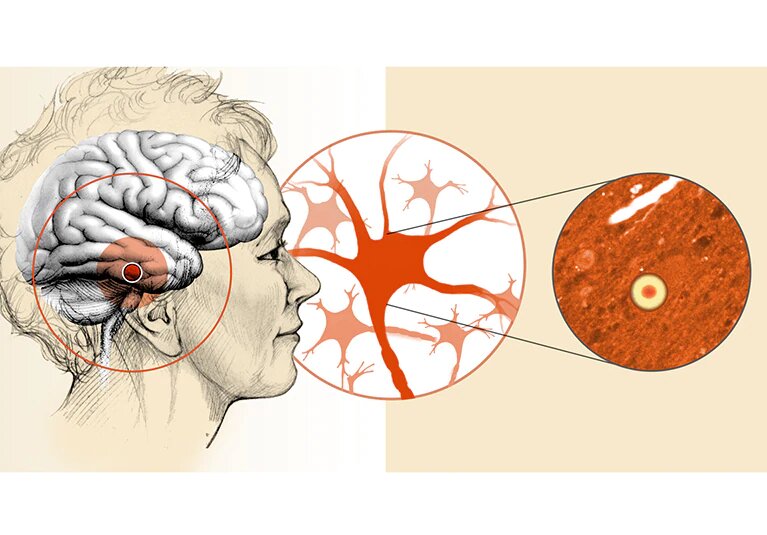
Lewy body dementia also called dementia with Lewy bodies, is the second most common kind of progressive dementia after Alzheimer’s disease dementia. Protein deposits, known as Lewy bodies, develop in nerve cells in the brain areas involved in thinking, memory, and movement (motor control).
Lewy body dementia leads to a progressive decrease in mental abilities. People with Lewy body dementia might experience visual hallucinations and changes in vigilance and attentiveness. Other effects include Parkinson’s disease-like signs and symptoms for example rigid muscles, slow movement, and tremors.
LEWY BODY DEMENTIA SYMPTOMS
Lewy body dementia signs and symptoms might include:
- Visual hallucinations – Hallucinations may be one of the first symptoms, and they usually recur. They might include seeing shapes, animals, or people that are not there. Sound (auditory), smell (olfactory), or touch (tactile) hallucinations can occur.
- Movement disorders – Signs of Parkinson’s disease (parkinsonian signs), for example, slowed movement, rigid muscles, tremors or a shuffling walk might happen. This could also result in falls.
Woman having difficulty in breathing - Poor regulation of body functions (autonomic nervous system) – Blood pressure, pulse, sweating, and the digestive process are regulated by a part of the nervous system that is usually affected by Lewy body dementia. This could result in dizziness, falls, and bowel problems for example constipation.
- Cognitive problems – You might experience thinking (cognitive) issues similar to those of Alzheimer’s disease, for example, confusion, poor attention, visual-spatial issues, and memory loss.
- Sleep difficulties – You might have rapid eye movement (REM) sleep behavior disorder, which could cause you to physically act out your dreams while you are asleep.
- Fluctuating attention – Episodes of sleepiness, long periods of staring into space, long naps at the time of the day, or disorganized speeches are possible.
- Depression – You might experience depression sometime during the course of your disease.
- Apathy – You might have a loss of motivation.
LEWY BODY DEMENTIA CAUSES
Lewy body dementia is characterized by the abnormal accumulation of proteins into masses called Lewy bodies. This protein is also related to Parkinson’s disease. People who have Lewy bodies in their brains also have plaques and tangles related to Alzheimer’s disease.
LEWY BODY DEMENTIA RISK FACTORS
A few factors seem to raise the risk of developing Lewy body dementia, including:
- Age – People older than 60 years are at greater risk.
- Sex – Lewy body dementia affects more males than females.
- Family history – Those who have a family member with Lewy body dementia or Parkinson’s disease are at higher risk.
LEWY BODY DEMENTIA COMPLICATIONS
Lewy body dementia is progressive. Signs and symptoms get worse, resulting in:
- Serious dementia
- Aggressive behavior
- Depression
- High risk of falling and injury
- Worsening of parkinsonian signs and symptoms, for example, tremors
- Death, on average about 8 years after symptoms start
LEWY BODY DEMENTIA DIAGNOSIS
A diagnosis of Lewy body dementia needs a progressive decrease in your ability to think, as well as two of the following:
- Fluctuating vigilance and thinking (cognitive) function
- Repeated visual hallucinations
- Parkinsonian symptoms
- REM sleep behavior disorder, in which people act out their dreams at the time of sleep
- Autonomic dysfunction, which involves instability of blood pressure and heart rate, poor regulation of body temperature, sweating, and
- associated symptoms, supports a Lewy body dementia diagnosis.
No single test could diagnose Lewy body dementia. Instead, doctors or primary care physicians diagnose your condition by ruling out other conditions that might cause similar signs and symptoms. Tests might include:
Neurological and physical exam
Your doctor or primary care physician might check for signs of Parkinson’s disease, strokes, tumors, or other medical conditions that could affect the brain and physical function. The neurological exam might test:
- Reflexes
- Strength
- Walking
- Muscle tone
- Eye movements
- Balance
- Sense of touch
- Pulmonary Edema
Evaluation of mental abilities
A short type of this test, which evaluates your memory and thinking skills, could be done in less than ten minutes in your doctor’s or primary care physician’s office. It is not usually useful in distinguishing Lewy body dementia from Alzheimer’s disease but could indicate dementia. Longer tests could take several hours, but help identify Lewy body dementia.
Your doctor or primary care physician will compare your test results with those of people of a similar age and education level. This could help distinguish normal from abnormal cognitive aging and might help diagnose the condition.
Blood tests
These could rule out physical problems that could affect brain function, for example, vitamin B-12 deficiency or an underactive thyroid gland.
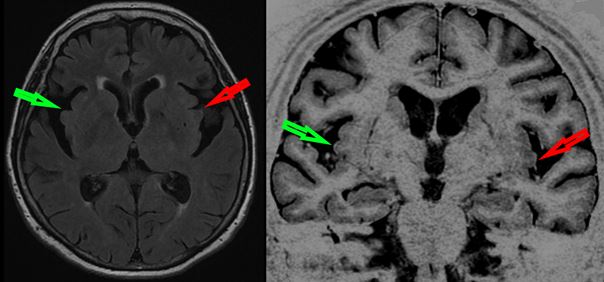
Brain scans
Your doctor or primary care physician might order an MRI or CT scan to identify a stroke or bleeding and to rule out the possibility of a tumor. While dementias are diagnosed based on the medical history and physical exam, specific features on imaging studies could suggest different forms of dementia, for example, Alzheimer’s or Lewy body dementia.
Most of the time, you would not require more brain scans. If the diagnosis is unclear or the signs and symptoms are not typical, your doctor or primary care physician might recommend some additional imaging tests, including these that could support a diagnosis of Lewy body dementia:
- Fluorodeoxyglucose PET brain scans, which could evaluate brain function.
- Single-photon emission computerized tomography (SPECT) or PET imaging, which could determine whether dopamine transporter uptake is lowered in the brain.
Your doctor or primary care physician might order a sleep evaluation to check for REM sleep behavior disorder or an autonomic function test to look for signs of heart rate and blood pressure instability.
Heart test
Your doctor or primary care physician might also order a heart test known as myocardial scintigraphy to check the blood flow to your heart, which could be a sign of Lewy body dementia.
LEWY BODY DEMENTIA TREATMENT
Treatment could be challenging, and there is no cure for Lewy body dementia. Doctors or primary care physicians treat the individual symptoms.
Medications
- Cholinesterase inhibitors – These Alzheimer’s disease medications, for example, rivastigmine (Exelon), donepezil (Aricept), and galantamine (Razadyne), work by increasing the levels of chemical messengers believed to be crucial for memory, thought, and judgment (neurotransmitters) in the brain. This could help improve vigilance and cognition and might help lower hallucinations and other behavioral issues.
- Possible side effects might include gastrointestinal upset, excessive salivation and tearing, and frequent urination. Donepezil is not approved by the Food and Drug Administration (FDA) for Lewy body dementia.
- In some people with moderate or severe dementia, an N-methyl-d-aspartate (NMDA)-receptor antagonist known as memantine (Namenda) might be added to the cholinesterase inhibitor.
- Parkinson’s disease medications – These medications, for example, carbidopa-levodopa (Sinemet, Rytary, Duopa) might help lower parkinsonian signs and symptoms, for example, rigid muscles and slow movement. Although, these medications might also increase confusion, hallucinations, and delusions.
- Medications to treat other symptoms – Your doctor or primary care physician might prescribe medications to treat other signs and symptoms related to Lewy body dementia, for example, sleep or movement problems.
If possible, avoid medications with anticholinergic properties, which could worsen cognition, or dopamine agonists, which could cause hallucinations.
First-generation antipsychotic medications, for example, haloperidol (Haldol), should not be used to treat Lewy body dementia. They might cause serious confusion, severe parkinsonism, sedation, and sometimes even death. Very infrequently, specific second-generation antipsychotics might be prescribed for a short time at a low dose but only if the benefits outweigh the risks.
Therapies
Because antipsychotic drugs could worsen Lewy body dementia symptoms, it may be helpful to first try non-drug approaches, for example:
- Tolerating the behavior – Many times a person with Lewy body dementia is not distressed by the hallucinations. In these cases, the side effects of medication might be worse than the hallucinations themselves.
- Modifying the environment – Lowering clutter and distracting noise could make it easier for someone with dementia to function.
- Providing soothing responses – A caregiver’s response might worsen behavior. Avoid correcting and quizzing a person with dementia. Provide reassurance and validation of his or her concerns.
- Creating daily routines and keeping tasks simple – Break tasks into easier steps and concentrate on successes, not failures. Structure and routine during the day could be less confusing.
If you or anyone you know is suffering from Lewy body dementia, our expert providers at Specialty Care Clinics will take care of your health and help you recover.
Call 469-545-9983 to book a telehealth appointment for an at-home check-up.