WHAT IS FIBROMUSCULAR DYSPLASIA?
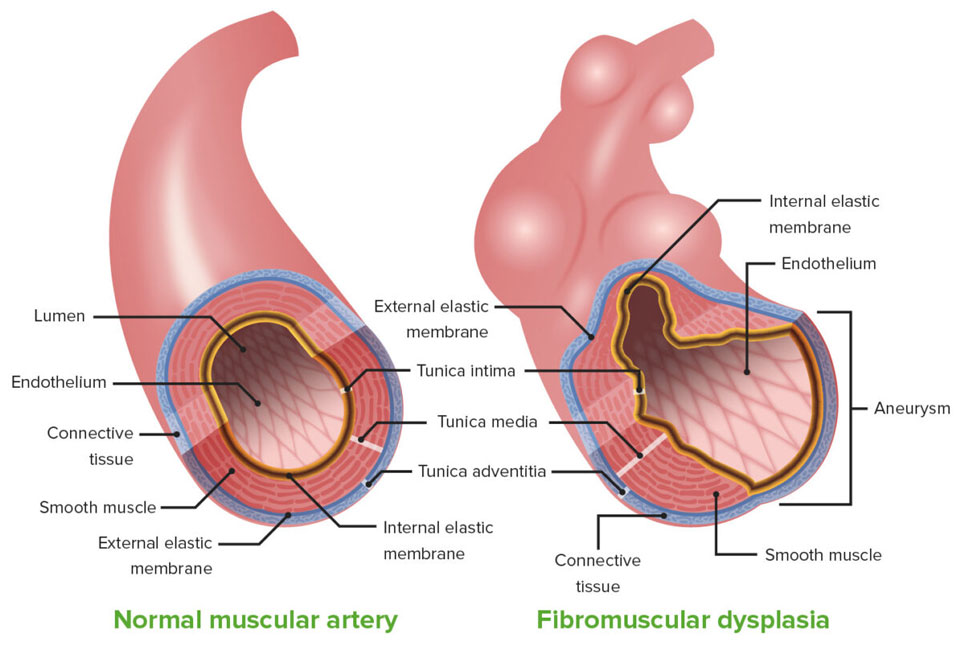
Fibromuscular dysplasia is a condition that causes the narrowing (stenosis) and enlargement (aneurysm) of the medium-sized arteries in your body. Narrowed arteries might decrease blood flow and affect the function of your organs.
Fibromuscular dysplasia appears most frequently in the arteries leading to the kidneys and brain. Fibromuscular dysplasia could affect other arteries, including those leading to your legs, heart, abdomen, and arms.
Treatments are available, but there is no cure for fibromuscular dysplasia.
FIBROMUSCULAR DYSPLASIA SYMPTOMS
Signs or symptoms of the disease depend on what artery is damaged by fibromuscular dysplasia. Sometimes, more than the artery is restricted. Many people who have fibromuscular dysplasia do not have any symptoms.
Kidney signs and symptoms
If the arteries leading to your kidneys (renal arteries) are affected, you might have:
- High blood pressure
- Tissue damage in your kidneys (ischemic renal atrophy)
- Chronic kidney failure (rarely)
Brain signs and symptoms
If the arteries leading to your brain (carotid arteries) are damaged, you might have:
- Headache
- Dizziness
- Temporary loss of vision
- Pulsating ringing in your ears (tinnitus)
- Neck pain
- Facial weakness or numbness
- Weakness or numbness in the limbs
- Trouble speaking
Abdominal signs and symptoms
If the arteries leading to your abdomen (mesenteric arteries) are damaged, you might have:
- Abdominal pain after eating
- Unintended weight loss
Heart signs and symptoms
Fibromuscular dysplasia usually happens with tears in the walls of your coronary arteries, also known as arterial dissection or spontaneous coronary artery dissection (SCAD). But the exact connection between these two conditions is not yet clear. If the arteries leading to your heart (coronary arteries) are damaged, you might have:
- Chest pain
- Shortness of breath
- Sweating
- Nausea
Leg and arm signs and symptoms
If the arteries leading to your arms or legs (peripheral arteries) are damaged, you might have:
- Uncomfortable when moving your legs, feet, arms, or hands
- Cold limbs
- Weakness
- Numbness
- Skin changes in color or appearance
WHEN SHOULD YOU SEE A DOCTOR?
If you have fibromuscular dysplasia, look for medical attention immediately if you have any of these signs and symptoms:
- Unexpected changes in your vision
- Unexpected changes in your ability to speak
- Unexpected or new weakness in your arms or legs
If you have any of the other signs or symptoms listed and are concerned about your risk of fibromuscular dysplasia, see your doctor or primary care physician.
Fibromuscular dysplasia could be passed down through families (inherited). Talk to your doctor or primary care physician about your family health history so together you could be alert to changes that may suggest you have fibromuscular dysplasia. There is currently no genetic test for fibromuscular dysplasia.
FIBROMUSCULAR DYSPLASIA CAUSES
The cause of fibromuscular dysplasia is not known. Although, several factors might play a role.
- Genetics – If someone in your family has fibromuscular dysplasia, you may get the condition, too. It may happen in a different artery or you might have a milder or more severe case. Or, you might never get fibromuscular dysplasia at all. Not all people with fibromuscular dysplasia have a relative with the disorder.
- Hormones – Women have fibromuscular dysplasia more usually than men do, so researchers think hormones might play a role in the development of the disease. But exactly how is not clear. Fibromuscular dysplasia is not connected to a woman’s use of birth control pills, the number of pregnancies, or the age when they gave birth.
- Abnormally formed arteries – A lack of oxygen to the arteries or the use of specific medications or tobacco could cause the arteries to develop abnormally, leading to decreased blood flow. Sometimes, the arteries might be positioned abnormally.
FIBROMUSCULAR DYSPLASIA RISK FACTORS
Several things could make you more likely to get fibromuscular dysplasia.
- Sex – Women have a much higher risk of fibromuscular dysplasia than do men.
- Age – Fibromuscular disease tends to be diagnosed in people in their early 50s.
- Smoking – If you are a smoker, quit smoking. People who smoke appear to have a high risk of developing fibromuscular dysplasia. For those already diagnosed with the disease, smoking increases the risk for more severe fibromuscular dysplasia.
FIBROMUSCULAR DYSPLASIA COMPLICATIONS
Fibromuscular dysplasia could cause a number of complications. These include:
- High blood pressure – A frequent complication of fibromuscular dysplasia is high blood pressure. The narrowing of the arteries causes higher pressure on your artery walls, which could lead to further artery damage, heart disease, or heart failure.
- Dissected artery – Fibromuscular dysplasia and tears in the walls of your arteries usually happen together. This process, known as arterial dissection or spontaneous coronary artery dissection (SCAD), could limit blood flow to the organ supplied by the injured artery. This could affect any artery.
- Aneurysms – Fibromuscular dysplasia could weaken the walls of your arteries, creating a bulge known as an aneurysm. If an aneurysm ruptures, it could be a life-threatening emergency. An aneurysm could happen in any artery affected by fibromuscular dysplasia.
- Stroke – If you have a dissected artery leading to your brain or if an aneurysm in an artery to your brain ruptures, you could have a stroke. High blood pressure could also increase your risk of a stroke.
FIBROMUSCULAR DYSPLASIA DIAGNOSIS
Because fibromuscular dysplasia might not cause any symptoms, it is unlikely your doctor or primary care physician would specifically check for this condition.
If someone in your family has or had fibromuscular dysplasia or aneurysm, your doctor or primary care physician might recommend checking you for fibromuscular dysplasia, too. Your doctor or primary care physician might check for fibromuscular dysplasia if he or she hears an abnormal sound in your upper stomach region that may be caused by an aneurysm.
Your doctor or primary care physician will perform a physical examination and order blood tests, including blood sugar and cholesterol levels, to check for signs of atherosclerosis, another condition that could narrow your arteries.
Tests to diagnose fibromuscular dysplasia can include:
- Duplex ultrasound – This non-invasive imaging test could determine if an artery is narrowed. During the test, an instrument known as a transducer is gently pressed to your skin. It transmits sound waves into your body. They bounce off the cells and body structures, showing how fast your blood flows and the size and shape of the blood vessels.
- Catheter-based angiography – During this frequently used test for fibromuscular dysplasia, a thin tube (catheter) is inserted into one of your arteries and moved until it reaches the location your doctor or primary care physician wants to examine. A small amount of dye is injected and X-rays are used to examine the location.
- Computerized tomography (CT) angiogram – A computerized tomography (CT) angiogram gives your doctor or primary care physician cross-sectional pictures of your body. It could detect narrowing in the arteries, aneurysms, and dissections. You lie down on a narrow table, which slides through a doughnut-shaped scanner. Before the test begins, you will receive an injection of a dye, which highlights regions of the body being examined.
- Magnetic resonance imaging (MRI) – Magnetic resonance imaging (MRI) uses a magnetic field and radio waves to create pictures of the body. It could see if you have an aneurysm or dissection. During the test, you will lie down on a narrow table that slides into a tube-like machine that is open on both ends.
The most frequent form of fibromuscular dysplasia looks like a “string of beads” on imaging tests. Other, more aggressive types of fibromuscular dysplasia have a smooth appearance.
Once you have been diagnosed with fibromuscular dysplasia, your doctor or primary care physician might repeat imaging tests from time to time to see if your signs and symptoms change or if your condition is getting worse.
FIBROMUSCULAR DYSPLASIA TREATMENT
Treatment for fibromuscular dysplasia depends on your health, the location of the narrowed artery, and other health conditions you have, like high blood pressure. Treatment alternatives include medications, medical procedures to improve blood flow, and surgery.
- Drugs
Treatment with high blood pressure medications is suggested for most people with fibromuscular dysplasia, even if they also have a procedure to correct the condition. Several different kinds of medications are available:
- Angiotensin-converting enzyme (ACE) inhibitors, like benazepril, enalapril, or lisinopril, help relax your blood vessels.
- Angiotensin II receptor blockers – These medications also help to relax your blood vessels. Instances of this class of medications include candesartan, irbesartan, losartan, and valsartan.
- Diuretics – These drugs, like hydrochlorothiazide, help remove excess fluid from your body and might be used with other blood pressure medications.
- Calcium channel blockers, like amlodipine, nifedipine, and others, helps to relax your blood vessels.
- Beta-blockers, like metoprolol, atenolol, and others, slow your heartbeat and block adrenaline.
Your doctor or primary care physician might also recommend you take a daily aspirin to lower your risk of stroke. But do not start taking an aspirin without talking to your doctor or primary care physician first.
Some of these medications used to treat fibromuscular dysplasia could affect the way your kidneys work. Your doctor or primary care physician might recommend blood and urine tests to make sure your kidneys are working normally once you start taking these medications.
-
- Procedures and surgery
- Percutaneous transluminal angioplasty (PTA)
- Procedures and surgery
This procedure is preferred over surgery and generally done at the same time as a catheter-based angiogram. During an angiogram, dye is administered through a catheter into an artery. X-rays show how the dye travels through the artery, revealing any narrowed regions. A wire is threaded to the artery and a catheter with a balloon is inserted in the narrowed region. The balloon is then inflated to open the restricted part of the artery. If your doctor or primary care physician finds severe damage associated with fibromuscular dysplasia, like an aneurysm, a metal mesh tube (stent) might be placed inside the weakened part of the artery to help prevent it from rupturing.
- Surgical revascularization
Surgery to repair the damaged artery is rarely suggested. It is usually only done when there are complications. Although, if percutaneous transluminal angioplasty (PTA) is not an option and the narrowing of your arteries is severe, your doctor or primary care physician might recommend a more invasive approach with surgery to repair or replace the narrowed portion of the artery. The type of surgery you will require depends on the location of the narrowed artery and how damaged the artery is.