WHAT IS ANGINA?
Angina is a kind of chest pain caused by decreased blood flow to the heart. Angina might be a symptom of coronary artery disease. Angina is otherwise known as angina pectoris.
Angina pain is usually described as squeezing, pressure, heaviness, tightness, or pain in the chest. It might feel like a heavy weight lying on the chest. Angina might be a new pain that needs to be checked by a health care provider or recurring pain that goes away with treatment.
Although angina is relatively common, it could still be hard to distinguish from other types of chest pain, like the discomfort of indigestion. If you have unexplained chest pain, seek medical help immediately.
TYPES
There are several types of anginas. The type depends on the cause and whether rest or medication eases symptoms.
- Stable angina – Stable angina is the most frequent form of angina. It generally happens during activity (exertion) and goes away with rest or angina medication. For example, pain that comes on when you are walking uphill or in the cold weather might be angina.
Stable angina pain is predictable and generally similar to previous episodes of chest pain. The chest pain generally lasts a short time, perhaps five minutes or less. - Unstable angina (a medical emergency) – Unstable angina is unpredictable and happens at rest. Or the angina pain is worsening and happens with less physical effort. It is typically severe and lasts longer than stable angina, maybe twenty minutes or longer. The pain does not go away with rest or the usual angina medications. If the blood flow does not improve, the heart is starved of oxygen and a heart attack happens. Unstable angina is dangerous and needs emergency treatment.
- Variant angina (Prinzmetal angina) – Variant angina, also known as Prinzmetal angina, is not due to coronary artery disease. It is caused by a spasm in the heart’s arteries that momentarily reduces blood flow. Severe chest pain is the primary symptom of variant angina. It most often occurs in cycles, generally at rest and overnight. The pain might be relieved by angina medication.
- Refractory angina – Angina episodes are common despite a combination of medications and lifestyle changes.
SYMPTOMS
Angina symptoms involve chest pain and discomfort. The chest pain or discomfort might feel like:
- Burning
- Fullness
- Pressure
- Squeezing
Pain might also be felt in the arms, neck, jaw, shoulder, or back.
Other symptoms of angina are:
- Dizziness
- Fatigue
- Nausea
- Shortness of breath
- Sweating
The severity, duration, and type of angina could vary. New or different symptoms might signal a more dangerous form of angina (unstable angina) or a heart attack.
Any new or worsening angina symptoms need to be evaluated immediately by a health care provider who could determine whether you have stable or unstable angina.
ANGINA IN WOMEN
Symptoms of angina in women could be different from the classic angina symptoms. These differences might lead to delays in seeking treatment. For example, chest pain is a common symptom in women with angina, but it might not be the only symptom or the most prevalent symptom for women. Women may also have symptoms like:
- Discomfort in the neck, jaw, teeth, or back
- Nausea
- Shortness of breath
- Stabbing pain rather than chest pressure
- Stomach (abdominal) pain
WHEN SHOULD YOU SEE A DOCTOR?
If your chest pain lasts longer than a few minutes and does not go away when you rest or take your angina medications, it might be a sign you are having a heart attack. Call 911 or emergency medical help immediately. Only drive yourself to the hospital unless there is no other transportation option.
If chest discomfort is a new symptom for you, it is important to see your health care provider to determine the cause and to get proper treatment. If you have been diagnosed with stable angina and it gets worse or changes, seek medical help right away.
CAUSES
Angina is caused by a decrease in blood flow into the heart muscle. Blood carries oxygen, which the heart muscle requires to survive. When the heart muscle is not getting enough oxygen, it causes a condition known as ischemia.
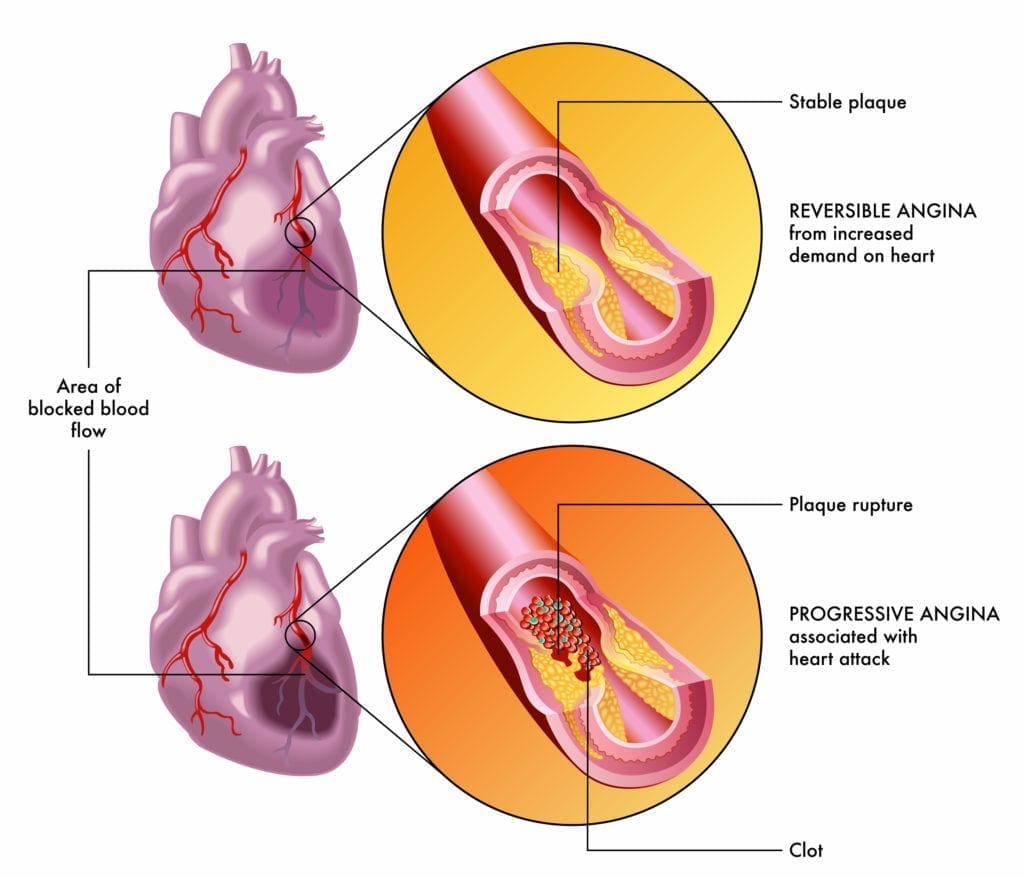
The most frequent cause of reduced blood flow to the heart muscle is coronary artery disease (CAD). The heart (coronary) arteries can become narrowed by fatty deposits known as plaques. This is known as atherosclerosis.
If plaques in a blood vessel rupture or a blood clot forms, it could quickly block or reduce flow through a narrowed artery. This could suddenly and severely decrease blood flow to the heart muscle.
During times of low oxygen demand — when resting, for example — the heart muscle might still be able to work on the reduced amount of blood flow without triggering angina symptoms. But when the demand for oxygen goes up, like when exercising, angina can result.
RISK FACTORS
The following things might increase the risk of angina:
- Increasing age – Angina is most common in adults aged 60 and older.
- Family history of heart disease – Inform your health care provider if your mother, father, or any siblings have had heart disease or a heart attack.
- Tobacco use – Smoking, chewing tobacco, and long-term exposure to secondhand smoke could damage the lining of the arteries, allowing deposits of cholesterol to collect and block blood flow.
- Diabetes – Diabetes increases the risk of coronary artery disease, which results in angina and heart attacks by speeding up atherosclerosis and increasing cholesterol levels.
- High blood pressure – With time, high blood pressure damages the arteries by accelerating the hardening of arteries.
- High cholesterol or triglycerides – Too much bad cholesterol — low-density lipoprotein (LDL) — in the blood could cause arteries to narrow. A high LDL raises the risk of angina and heart attacks. A high level of triglycerides in the blood also is not healthy.
- Other health conditions – Chronic kidney disease, peripheral artery disease, metabolic syndrome, or a history of stroke raises the risk of angina.
- Not enough exercise – An inactive lifestyle contributes to high cholesterol, high blood pressure, type two diabetes, and obesity. Speak to your health care provider about the type and amount of exercise that is best for you.
- Obesity – Obesity is a risk factor for heart disease, which could cause angina. Being overweight makes the heart work difficult to supply blood to the body.
- Emotional stress – Too much stress and anger could raise blood pressure. Surges of hormones produced during stress could narrow the arteries and worsen angina.
- Medications – Drugs that tighten blood vessels, like some migraine drugs, might trigger Prinzmetal’s angina.
- Drug misuse – Cocaine and other stimulants could cause blood vessel spasms and trigger angina.
- Cold temperatures – Exposure to cold temperatures could trigger Prinzmetal angina.
COMPLICATIONS
The chest pain that occurs with angina can make doing some activities, like walking, uncomfortable. However, the most serious complication is a heart attack.
Early warning signs and symptoms of a heart attack are:
- Pressure, fullness, or a squeezing pain in the middle of the chest that lasts for more than a few minutes
- Pain that spreads beyond the chest to the shoulder, arm, back, or even to the teeth and jaw
- Fainting
- An impending sense of doom
- Increasing episodes of chest pain
- Nausea and vomiting
- Continuous pain in the upper belly area (abdomen)
- Shortness of breath
- Sweating
If you experience any of these symptoms, look for emergency medical attention right away.
PREVENTION
You could help prevent angina by following the same lifestyle changes that are used to treat angina. These include:
- Not smoking
- Eating a healthy diet
- Avoiding or limiting alcohol
- Exercising regularly
- Maintaining a healthy weight
- Managing other health conditions associated with heart disease
- Reducing stress
- Getting recommended vaccines to prevent heart complications
DIAGNOSIS
To diagnose angina, your health care provider will do a physical examination and ask questions about your symptoms. You will also be asked about any risk factors, including whether you have a family history of heart disease.
Tests used to diagnose and confirm angina are:
- Electrocardiogram (ECG or EKG) – This quick and pain-free test measures the electrical activity of the heart. Sticky patches (electrodes) are placed on the chest and at times the arms and legs. Wires join the electrodes to a computer, which shows the test results. An ECG could show if the heart is beating too fast, too slow, or not at all. Your health care provider also could look for patterns in the heart rhythm to see if blood flow through the heart has been slowed or interrupted.
- Chest X-ray – A chest X-ray displays the condition of the heart and lungs. A chest X-ray might be done to determine if other conditions are causing chest pain symptoms and to see if the heart is enlarged.
- Blood tests – Specific heart enzymes enter the bloodstream when the heart muscle is damaged, such as from a heart attack. A cardiac enzyme blood test could help detect these substances.
- Stress test – At times angina is easier to diagnose when the heart is working harder. A stress test typically includes walking on a treadmill or riding a stationary bike while the heart is monitored. Other tests might be done at the same time as a stress test. If you cannot exercise, you may be given drugs that mimic the effect of exercise on the heart.
- Echocardiogram – An echocardiogram uses sound waves to produce pictures of the heart in motion. These pictures can show how blood flows through the heart. An echocardiogram might be done during a stress test.
- Nuclear stress test – A nuclear stress test helps to measure blood flow into the heart muscle at rest and during stress. It is similar to a routine stress test, but during a nuclear stress test, a radioactive tracer is administered into the bloodstream. A special scanner displays how the tracer moves through the heart arteries. Areas that have little or no amounts of the tracer indicate poor blood flow.
- Cardiac computerized tomography (CT) – For this test, you typically lie down on a table inside a doughnut-shaped machine. An X-ray tube inside the machine rotates around the body and collects pictures of the heart and chest. A cardiac CT scan could show if the heart is enlarged or if any heart’s arteries are narrowed.
- Cardiac magnetic resonance imaging (MRI) – This test uses magnetic fields and radio waves to create detailed pictures of the heart. You typically lie down on a table inside a long, tubelike machine that produces detailed pictures of the heart’s structure and blood vessels.
- Coronary angiography – Coronary angiography uses X-ray imaging to check the inside of the heart’s blood vessels. It is part of a general group of procedures called cardiac catheterization.
A health care provider threads a thin tube (catheter) through a blood vessel in the arm or groin to an artery in the heart and administers dye through the catheter. The dye makes the heart arteries appear more clearly on an X-ray. Your health care provider may call this type of X-ray an angiogram.
TREATMENT
Options for angina treatment are:
- Lifestyle changes
- Medications
- Angioplasty and stenting
- Open-heart surgery (coronary bypass surgery)
The goals of angina treatment are to decrease the frequency and severity of the symptoms and to lower the risk of a heart attack and death.
You will need immediate treatment if you have unstable angina or angina pain that’s different from what you generally have.
Medications
If lifestyle changes — like eating healthy and exercising — do not improve heart health and relieve angina pain, medications might be needed. Medications to treat angina might include:
- Nitrates – Nitrates are frequently used to treat angina. Nitrates relax and broaden the blood vessels so more blood flows to the heart. The most frequent form of nitrate used to treat angina is nitroglycerin. The nitroglycerin pill is placed below the tongue. Your health care provider may recommend taking a nitrate before activities that typically trigger angina (such as exercise) or on a long-term preventive basis.
- Aspirin – Aspirin lowers blood clotting, making it easier for blood to flow through narrowed heart arteries. Preventing blood clots could reduce the risk of a heart attack. Do not start taking a daily aspirin without talking to your health care provider first.
- Clot-preventing drugs – Certain medications such as clopidogrel (Plavix), prasugrel (Effient), and ticagrelor (Brilinta) make blood platelets less likely to stick together, so blood does not clot. One of these medications might be recommended if you cannot take aspirin.
- Beta-blockers – Beta-blockers cause the heart to beat more slowly and with less force, which reduces blood pressure. These medications also relax blood vessels, which improves blood flow.
- Statins – Statins are drugs used to decrease blood cholesterol. High cholesterol is an important risk factor for heart disease and angina. Statins block a substance that the body requires to make cholesterol. They help prevent obstructions in the blood vessels.
- Calcium channel blockers – Calcium channel blockers, also known as calcium antagonists, relax and broaden blood vessels to improve blood flow.
- Other blood pressure medications – Other drugs to reduce blood pressure include angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs). If you have high blood pressure, diabetes, signs of heart failure, or chronic kidney disease, your health care provider might prescribe one of these types of medications.
- Ranolazine (Ranexa) – This medication might be prescribed for chronic stable angina that does not get better with other medications. It might be used alone or with other angina medications, such as calcium channel blockers, beta-blockers, or nitroglycerin.
Therapies
Sometimes, a nondrug option known as enhanced external counterpulsation (EECP) may be recommended to increase blood flow to the heart. With EECP, blood pressure-type cuffs are positioned around the calves, thighs, and pelvis. EECP needs multiple treatment sessions. EECP might help reduce symptoms in people with frequent, uncontrolled angina (refractory angina).
Surgery and procedures
If lifestyle changes, medications, or other therapies do not reduce angina pain, a catheter procedure or open-heart surgery might be needed.
Surgeries and procedures used to treat angina and coronary artery disease are:
- Angioplasty with stenting – During an angioplasty — also known as a percutaneous coronary intervention (PCI) — a tiny balloon is inserted into the narrowed artery. The balloon is inflated to widen the artery, and then a small wire mesh coil (stent) is generally inserted to keep the artery open.
Angioplasty with stenting improves blood flow to the heart, reducing or eliminating angina. Angioplasty with stenting might be a good treatment option for those with unstable angina or if lifestyle changes and medications do not effectively treat chronic, stable angina. - Open-heart surgery (coronary artery bypass surgery)– During coronary artery bypass surgery, a vein or artery from somewhere else in the body is used to bypass an obstructed or narrowed heart artery. Bypass surgery raises blood flow to the heart. It is a treatment option for both unstable angina and stable angina that has not responded to other treatments.
If you or anyone you know is suffering from angina our expert providers at Specialty Care Clinics will take care of your health and help you recover.
Call 469-545-9983 to book a telehealth appointment for an at-home check-up.