WHAT IS MAIGNE’S SYNDROME?
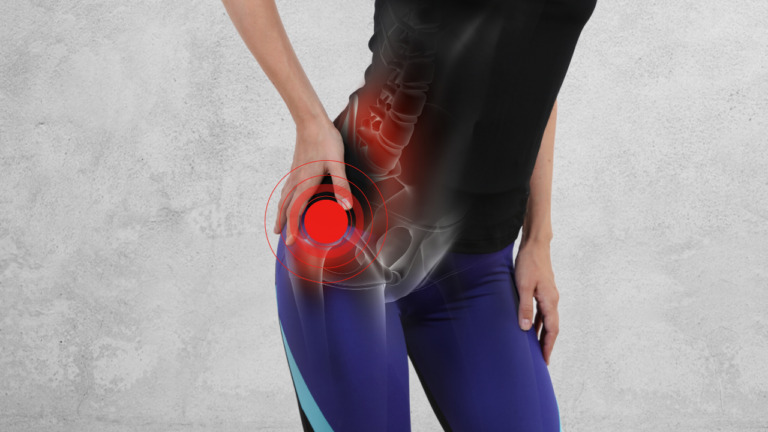
Maigne syndrome is a frequently ignored source of the lower back, hip, and crotch inconvenience. Spinal dysfunction prompting pain and degeneration is normal at temporary destinations like the thoracolumbar intersection (TLJ). The sagittally-adjusted lumbar features limit revolution. Conversely, the thoracic spine pivots substantially more uninhibitedly because of the front-facing plane arrangement of its features. Revolution and supported flexion force pressure to this area. Bothering frequently influences the essential back ramus of the TLJ, bringing about transmitting symptoms, or Maigne Syndrome. Patients with Maigne Syndrome normally present with essential hip and crotch pain, incidentally joined by LBP. Symptoms may likewise allude to the lower midsection, pubic locale, iliac fossa, back iliac peak, butt cheek, testicle, or labia.

WHAT LEADS TO MAIGNE’S SYNDROME?
What happens in Maigne’s syndrome is that development is decreased in the progress region of the spine, where the principal lumbar vertebra and last thoracic vertebrae are associated. Lumbar vertebrae aren’t fit to pivot or turn like the thoracic vertebrae are, making the site vulnerable to issues. Spinal unsteadiness or joint degeneration might be contributing elements in the improvement of Maigne’s syndrome.
With Maigne’s syndrome, the pain most often presents just on one side (one-sided) of the spine and once in a long while, if at any point, influences the two sides at the same time. Moreover, victims of the syndrome never whine of pain influencing the TLJ itself. The example of pain, as a rule, emanates along the pathway of the impacted nerves leaving the TLJ.
A huge reason behind Maigne’s syndrome eludes medical experts is that the pain related to the condition rarely presents at the source of the tissue harm, irritation, or potential dysfunction. All things considered, the pain is ‘referred’ along the length of the impacted nerve and presents somewhere else in the body, normally considerably more distally (away from the spine) in regions like the hip, external thigh, and crotch. Hip and crotch pain can frequently be an exemplary side effect of Maigne’s syndrome.
HOW TO IDENTIFY MAIGNE’S SYNDROME?
Referred pain, which is otherwise called radicular pain, happens when the painful symptoms present in one region of the body as an immediate aftereffect of an improvement, aggravation, or dysfunction somewhere else. With Maigne’s syndrome, the most well-known symptoms include:
- Pain in the lower back district, regularly around the SI joint
- Pain in the crotch or privates
- Lower stomach pain
- Pain in the pubic bone
- Pain in the lumbo-sacral district
- Groin pain
- Testicular pain
- Abdominal pain
- Gynecological pain
- Pubic bone pain
- Aching or painful sensation radiating above.
- Pain along the pelvis and into the pubic region.
- Buttock pain
- On the side of the hip (trochanteric bursitis)
Since the nerves in the thoracolumbar intersection feed the flank, hip, and crotch, Maigne’s syndrome regularly gives itself a pain in the lower back or spine, which might emanate across the lumbar district and into the hip. Whenever fringe cluneal nerve entanglement happens, constant standing and additionally strolling may disturb symptoms, which are frequently confused with lumbar stenosis.

HOW TO DIAGNOSE MAIGNE’S SYNDROME?
If you have pain in any of the above areas the doctor would have a test of the whole spinal section including palpation of the features and spinous cycles for any expectations of deciding the degree of origin. Secondly, the patient won’t ordinarily have unconstrained pain at the culpable spinal level. Pain can be incited by palpation of the aspect joints, or the level can stay hidden, with just the referred pain as proof of the deformity. Generally one-sided, two-sided cases have been depicted as we present here. Patients won’t have pain transmitting beneath the knee, which is more average for the foremost ramus association.
Third, the radiographic proof is non-contributory. X-ray, CT, and myelography are largely insufficient at restricting the blame level. The run-of-the-mill degenerative changes seen in most pictures might prompt superfluous medical procedures or bogus determination. The back ramus is distant from herniating or swelling circles.
The fourth measure secures the finding: pain let by infusion free from neighborhood sedative into the right feature joint. This analytic methodology can likewise be remedial; the infusion of steroids or radiofrequency denervation of the average branch can be added for stubborn cases.
TREATMENT AND MANAGEMENT OF MAIGNE’S SYNDROME
While Maigne’s syndrome can be challenging to analyze for medical services experts who aren’t acquainted with it, most alignment specialists can pinpoint and treat the issue. The proposed treatment plan will rely upon whether the issue is because of precariousness (hypermobility) or degeneration (hypomobility) nearby. Hypermobility methodologies will zero in on acquiring dependability, while hypomobility issues might require treatment that opens the intervertebral foramen.

- Neural Desensitization Maneuvers: These techniques release local adhesions of the cluneal nerves at the thoracolumbar aponeurosis. Brain preparation streamlines the capacity of mechanical points of interaction to skim comparative with the brain structure. Dynamic and inactive extending reduces intraneural edema and tension by assembling the fringe nerve as well as related vascular designs.
- Injections: The allopathic moderate methodology for cluneal nerve ensnarement incorporates a sedative nerve square and calming steroid infusions. If these treatment approaches are fruitless, surgery might follow.
OUTLOOK
Maigne’s syndrome normally presents as one-sided pain in the lower horizontal area of the spine, crotch pain, and additionally a throbbing or painful vibe that emanates above and along the pelvis and into the pubic locale.
If you or anyone you know is suffering from a lower back pain, our expert providers at Specialty Care Clinics will take care of your health and help you recover.
Call us on (469) 545-9983 to book an appointment with our specialists.
