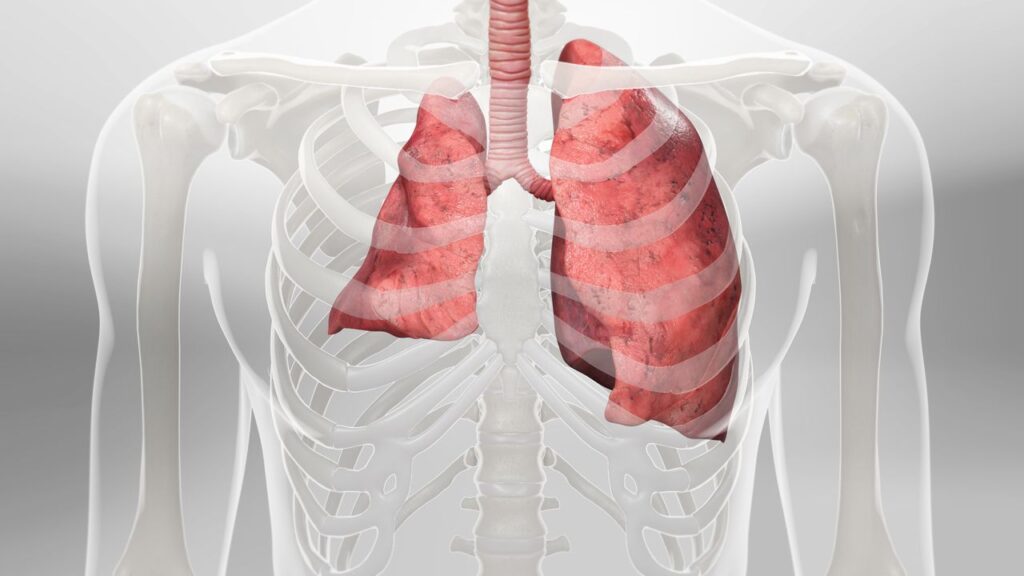
RARE LUNG CONDITION: PNEUMOTHORAX OR COLLAPSED LUNG
In a healthy body, the lungs are contacting the walls of the chest. A pneumothorax or collapsed lung happens when air gets into the space between the chest wall and the lung, called the pleural space. The pressure of this air makes the lung break down on itself. The lung may completely fall, however, most frequently just a piece of its breakdowns. This breakdown can likewise come down on the heart, bringing on additional side effects.
There can be numerous things that cause pneumothorax, and symptoms can fluctuate generally. Specialists can assist with diagnosing and treating pneumothorax.
WHAT IS PNEUMOTHORAX OR COLLAPSED LUNGS?
A collapsed lung or medicinally known as pneumothorax happens when air enters the pleural space, the region between the chest wall and the lung. Air in the pleural space can develop and press against the lung, making it break down partially or completely.
Pneumothorax can be traumatic or non-traumatic.
- Traumatic pneumothorax results from a physical issue, similar to a catastrophe for the chest.
- Non-traumatic pneumothorax can occur assuming you have lung sickness, like chronic obstructive pneumonic illness (COPD), yet it can likewise occur for reasons unknown in individuals without lung illness.
The long-term effect of pneumothorax can fluctuate. If by some stroke of good luck a limited quantity of air is caught in the pleural space, there might be no further entanglements. Assuming that the volume of air is more enormous or it influences the heart, it very well may life-compromise.
WHAT LEADS TO COLLAPSED LUNGS?
Collapsed lungs or pneumothorax are usually caused by three main reasons, which include medical conditions, injuries, and lifestyle factors.
Medical conditions:
Some of the common medical conditions that may lead to a collapsed lung include:
- Asthma.
- Pneumonia.
- Collagen vascular disease.
- Chronic obstructive pulmonary disease (COPD).
- Cystic fibrosis.
- Idiopathic pulmonary fibrosis.
- Emphysema.
- Endometriosis in the chest.
- Lung cancer.
- Lymphangioleiomyomatosis.
- Marfan syndrome.
- Tuberculosis.
- Acute respiratory distress syndrome (ARDS).
- Coronavirus infection.
Injuries:
Accidents or other wounds may sometimes lead to a collapsed lung. Such as:
- Blunt force trauma.
- Some types of ventilation or changes to ventilation.
- Gunshot wound.
- Lung puncture during a medical procedure, such as biopsy or nerve block.
- Stab wound.
Lifestyle factors:
Your lifestyle choices may also lead to a collapsed lung. Such as:
- Use of Drugs, especially drugs that are inhaled.
- Smoking.
- Flying involves drastic changes in air pressure.
- Scuba or deep-sea diving.
Sometimes people with other risk factors may also develop a collapsed lung. These are:
- Family history of pneumothorax.
- Pregnancy.
- Tall, thin body type.
WHAT ARE THE SYMPTOMS OF COLLAPSED LUNGS?
A collapsed lung can have different signs and symptoms. At first, Symptoms of pneumothorax may scarcely be perceptible from the start and can be mistaken for different issues.
The symptoms of pneumothorax can vary from mild to life-threatening and may include:
- Shortness of breath
- Chest pain, which may be more severe on one side of the chest
- Sharp pain when inhaling
- Pressure in the chest that gets worse over time
- Blue discoloration of the skin or lips
- Increased heart rate
- Rapid breathing
- Confusion or dizziness
- Coma or loss of consciousness
A few cases of pneumothorax have no visible symptoms. These must be diagnosed with the help of an X-ray or one more kind of scan. Others may require immediate medical attention. If you are experiencing the symptoms above you should contact your healthcare provider or seek immediate medical care.
ARE YOU AT HIGH RISK OF DEVELOPING COLLAPSED LUNG?
The risk factors vary for a traumatic and spontaneous pneumothorax.
- Traumatic pneumothorax: The risk factors include:
1. Contact sports, such as hockey or football.
2. Working in an environment involving a risk of falls or other types of injury.
3. A medical procedure involving the chest or lung area.
4. Ongoing respiratory care. - Spontaneous pneumothorax: You are at the highest risk of a non-traumatic pneumothorax when:
1. You have a history of smoking.
2. You have an existing lung condition, such as asthma or COPD.
3. You have a family history of pneumothorax.
4. You have tall, slim bodies, affecting pressure at the top of the lung.
5. You have inflammation in the small airways.
HOW DO DOCTORS DIAGNOSE COLLAPSED LUNG?
Your medical services supplier will get some information about your set of experiences of lung infection and play out an actual exam. They may likewise quantify the level of specific gases in your circulation system. To measure gases such as oxygen and carbon dioxide, an expert gathers a blood test and breaks down it in a lab.
The most widely recognized method for diagnosing a collapsed lung is clinical imaging. Generally, you’ll have a chest X-ray. However, you might have a CT output or ultrasound.
HOW TO TREAT COLLAPSED LUNG PROBLEM?
Most types of pneumothorax require clinical consideration. The extent of this clinical consideration can fluctuate as much as the actual problem. The standard clinical treatment for the most part includes embedding a little cylinder between the ribs or under the collarbone to deliver the gas that has developed. This will gradually de-pressurize the lung.
Specialists might recommend different medications to numb agony, assist with eliminating toxins, or forestall disease in the body. Certain individuals might require oxygen assuming that their lung limit is lacking. Careful treatment might be fundamental at times, particularly in people who have had rehashed pneumothoraces.
The treatment regime for collapsed lung may include:
- Observation: In cases of minor pneumothorax, your provider shall watch for signs of heart or breathing problems.
Supplemental oxygen: You may require extra oxygen if your pneumothorax is small and you are showing symptoms. Your doctor would keep you under observation until your condition is stable. - Needle aspiration: During aspiration, your doctor removes a portion of the air in the pleural space with the help of a needle. The specialist might follow needle aspiration with percutaneous chest tube drainage.
- Chest tube drainage: In the event of a larger pneumothorax, your supplier might place an empty cylinder in your chest to decrease the air in the pleural space. As the pneumatic force diminishes, the lung re-expands and heals.
- Chemical pleurodesis: To prevent the lung from imploding once more, a supplier might perform pleurodesis. Your doctor cuts and inserts a tube. Then, at that point, your doctor utilizes chemicals (like doxycycline or powder) to attach the lung to the chest cavity, eliminating extra space in the chest cavity.
- Surgery: Video-assisted thoracoscopic surgery (VATS) is a minimally invasive procedure utilizing a small camera to help the surgeon remove lung tissue. Your specialist may likewise play out synthetic pleurodesis or mechanical pleurodesis utilizing a piece of cloth to connect the lung to the chest cavity.
You may require surgery if you don’t respond to other treatments or have:
- Persistent air leakage from chest tube.
- A lung that does not expand despite chest tube insertion.
- Recurrent collapsed lung.
- Pneumothorax in both lungs.
- Traumatic lung injuries.
OUTLOOK
A collapsed lung is rare, however, it can be a serious condition. If you have signs or symptoms of a collapsed lung, such as chest pain or inconvenience in breathing, get medical care immediately. Your lung might have the option to heal on its own, or you might require treatment to save your life. Your doctor can determine the best type of treatment for you.
People Also Read:
- Pleural Effusion – Causes, Symptoms and Treatment
- Interstitial Lung Disease – Causes, Symptoms and Treatment
If you or anyone you know is suffering from pneumothorax , our expert providers at Specialty Care Clinics will take care of your health and help you recover.
Call us on (469) 545-9983 to book an appointment with our specialists.