WHAT IS REACTIVE ARTHRITIS?
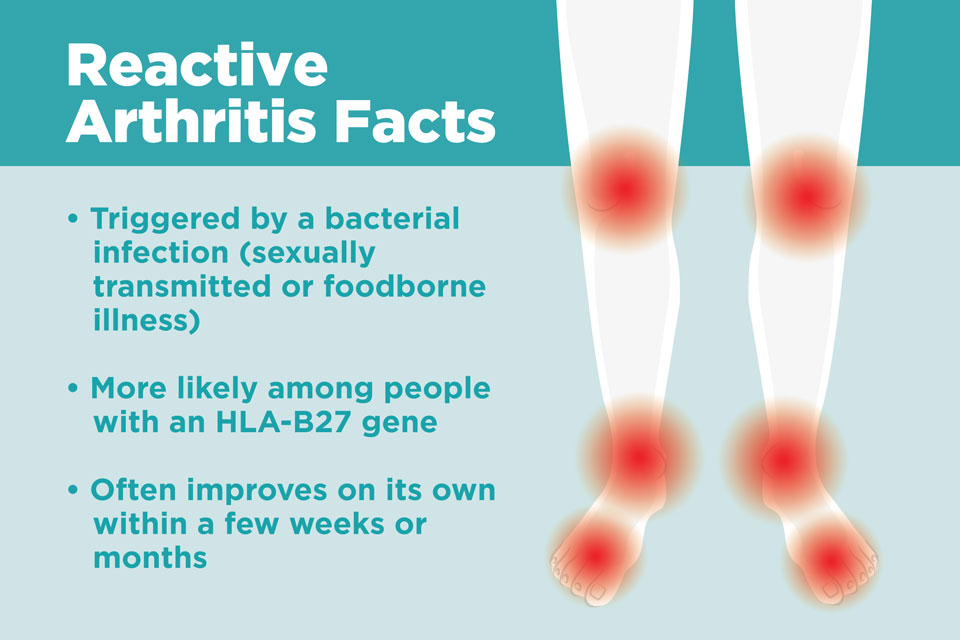
Reactive arthritis is joint pain and swelling triggered by an infection in another part of the body — most frequently the intestines, genitals, or urinary tract.
This condition generally targets the knees, ankles, and feet. Inflammation also could affect the eyes, skin, and the tube that carries urine out of the body (urethra). Previously, reactive arthritis was sometimes known as Reiter’s syndrome.
SYMPTOMS
The signs and symptoms of reactive arthritis generally begin one to four weeks after exposure to a triggering infection. They may include:
- Pain and stiffness – The joint pain associated with reactive arthritis most commonly happen in the knees, ankles, and feet. Pain might also occur in the heels, low back, or buttocks.
- Eye inflammation – Many people who suffer from reactive arthritis also develop eye inflammation (conjunctivitis).
- Urinary problems – Increased frequency and discomfort during urination might occur, as can inflammation of the prostate gland or cervix.
- Inflammation of tendons and ligaments where they attach to bone (enthesitis) – This happens most frequently in the heels and the sole of the feet.
- Swollen toes or fingers – In some cases, toes or fingers may become so swollen that they look like sausages.
- Low back pain – The pain tends to get worse at night or in the morning.
WHEN SHOULD YOU SEE A DOCTOR?
If you develop joint pain within one month of having diarrhea or genital infection, contact your healthcare provider.
CAUSES
Reactive arthritis develops in reaction to an infection in your body, usually in your intestines, genitals, or urinary tract. You may not be aware of the triggering infection if it causes mild symptoms or none at all.
Numerous bacteria could cause reactive arthritis. Some are transmitted sexually, and others are foodborne. The most common ones are:
- Campylobacter
- Chlamydia
- Clostridioides difficile
- Escherichia coli
- Salmonella
- Shigella
- Yersinia
Reactive arthritis is not contagious. However, the bacteria that cause it could be transmitted sexually or in contaminated food. Only a few people who are exposed to the bacteria develop reactive arthritis.
RISK FACTORS
Specific factors increase your risk of reactive arthritis:
Sudden (acute) pulmonary edema symptoms:
- Age – Reactive arthritis happens most frequently in adults between the ages of 20 and 40.
- Sex – Women and men are just as likely to develop reactive arthritis in response to foodborne infections. Although, men are more likely than women to develop reactive arthritis in response to sexually transmitted bacteria.
- Hereditary factors – A particular genetic marker has been linked to reactive arthritis. But the majority of people who have this marker never develop the condition.
PREVENTION
Genetic factors appear to play a role in whether you are likely to develop reactive arthritis. Though you cannot change your genetic makeup, you can reduce your exposure to bacteria that may lead to reactive arthritis.
Store your food at the correct temperatures and cook it properly. Doing these things help you avoid the many foodborne bacteria that could cause reactive arthritis, including salmonella, shigella, yersinia, and campylobacter. Some sexually transmitted infections could trigger reactive arthritis. Use condoms to help reduce your risk.
DIAGNOSIS
During the physical examination, your doctor is likely to check your joints for swelling, warmth, and tenderness, and test the range of motion in your spine and affected joints. Your doctor may also check your eyes for inflammation and your skin for rashes.
Blood tests
Your doctor may recommend that a sample of your blood be tested for:
- Evidence of past or current infection
- Signs of inflammation
- Antibodies related to other types of arthritis
- A genetic marker connected to reactive arthritis
Joint fluid tests
Your doctor may use a needle to withdraw a sample of fluid from within an affected joint. This fluid will be tested for:
- White blood cell count – An increased number of white blood cells may indicate inflammation or an infection.
- Infections – Bacteria in your joint fluid may indicate septic arthritis, which can result in severe joint damage.
- Crystals – Uric acid crystals in your joint fluid may indicate gout. This very painful type of arthritis usually affects the big toe.
Imaging tests
X-rays of your low back, pelvis, and joints could indicate whether you have any of the characteristic signs of reactive arthritis. X-rays could also rule out other types of arthritis.
TREATMENT
The goal of treatment is to manage your symptoms and treat an infection that can still be present.
Medications
If your reactive arthritis was triggered by a bacterial infection, your doctor may prescribe an antibiotic if there is evidence of persistent infection. Which antibiotic you take depends upon the bacteria that are present.
Signs and symptoms of reactive arthritis might be eased with:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) – Prescription NSAIDs, like indomethacin (Indocin), can relieve the inflammation and pain of reactive arthritis.
- Steroids – A steroid injection into affected joints could reduce inflammation and allow you to return to your usual activity level. Steroid eye drops might be used for eye symptoms, and steroid creams might be used for skin rashes.
- Rheumatoid arthritis drugs – Limited evidence suggests that medications like sulfasalazine (Azulfidine), methotrexate (Trexall), or etanercept (Enbrel) can relieve pain and stiffness for some people with reactive arthritis.
Physical therapy
A physical therapist could provide you with targeted exercises for your joints and muscles. Strengthening exercises increase the joint’s support by developing the muscles around the damaged joints. Range-of-motion exercises could increase your joints’ flexibility and reduce stiffness.
If you or anyone you know is suffering from reactive arthritis, our expert providers at Specialty Care Clinics will take care of your health and help you recover.
Call us on 469-545-9983 to book an appointment with our specialists.