WHAT IS LYMPHEDEMA?
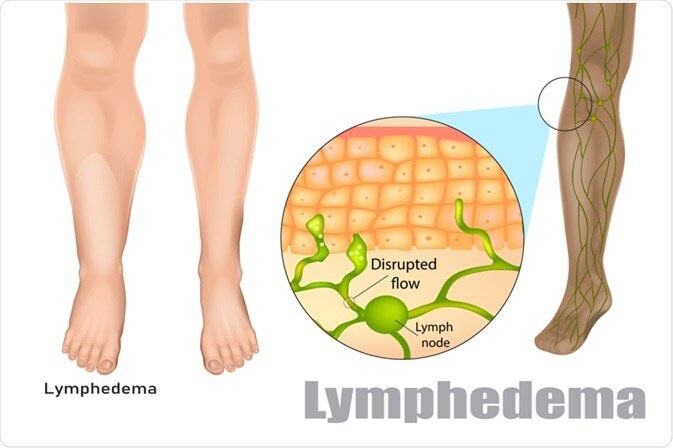
Lymphedema refers to swelling that usually happens in one of your arms or legs. Sometimes both arms and legs swell.
Lymphedema is most frequently caused by the removal of or damage to your lymph nodes as a part of cancer treatment. It is caused by a blockage of your lymphatic system that is part of your immune system. The blockage prevents lymph fluid from draining properly, and the fluid build-up leads to inflammation.
While there is presently no cure for lymphedema, it could be managed with early diagnosis and diligent care of your damaged limb.
LYMPHEDEMA SYMPTOMS
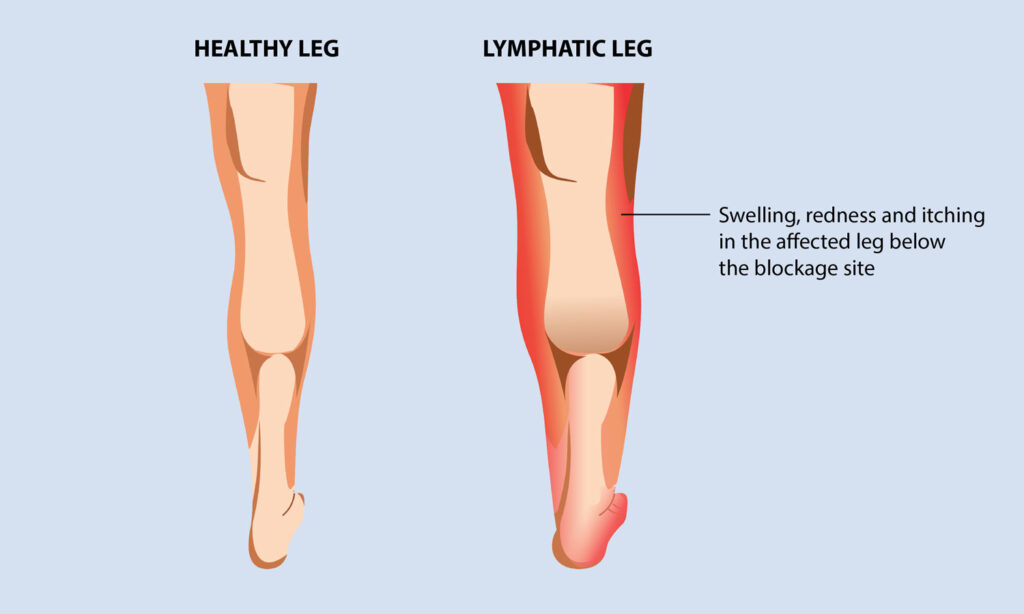
Lymphedema signs and symptoms, which happen in your affected arm or leg, include:
- Inflammation of part or all of your arm or leg, including fingers or toes
- A sensation of heaviness or tightness
- Limited range of motion
- Aching or discomfort
- Recurring infections
- Hardening and thickening of the skin (fibrosis)
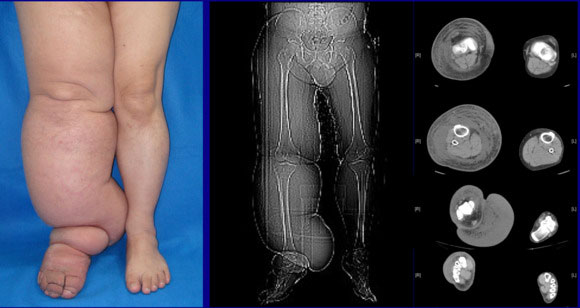
The inflammation caused by lymphedema ranges from mild, hardly noticeable changes in the size of your arm or leg to extreme changes that make the limb difficult to use. Lymphedema caused by cancer treatment can take place only months or years after treatment.
WHEN SHOULD YOU SEE A DOCTOR?
Make an appointment with your doctor or primary care physician if you notice persistent swelling in your arm or leg.
If you already have the diagnosis of lymphedema of a limb, see your doctor or primary care physician if there is an unexpected dramatic increase in the size of the involved limb, as it might suggest a new process is occurring.

LYMPHEDEMA CAUSES
Your lymphatic system is important to keeping your body healthy. It circulates protein-rich lymph liquid in every part of your body, collecting bacteria, viruses, and waste products. Your lymphatic system carries this fluid and harmful substances across your lymph vessels, which lead to lymph nodes. The wastes are then filtered out by lymphocytes infection-fighting cells that live in your lymph nodes and are eventually flushed from your body.
Lymphedema happens when your lymph vessels are unable to adequately drain lymph fluid, generally from an arm or leg. Lymphedema could be either primary or secondary. This means it could happen on its own (primary lymphedema), or be caused by another disease or condition (secondary lymphedema). Secondary lymphedema is far more frequent than primary lymphedema.
CAUSES OF SECONDARY LYMPHEDEMA
Any condition or procedure that damages your lymph nodes or lymph vessels could cause lymphedema. Causes include:
- Surgery – Removal of or injury to lymph nodes and lymph vessels might result in lymphedema. For instance, lymph nodes might be removed to check for the spread of breast cancer, and lymph nodes might be injured in surgery that involves blood vessels in your limbs.
- Radiation treatment for cancer – Radiation could cause scarring and swelling of your lymph nodes or lymph vessels.
- Cancer – If cancer cells block lymphatic vessels, lymphedema might result. For example, a tumor growing near a lymph node or lymph vessel can enlarge enough to block the flow of the lymph fluid.
- Infection – An infection of the lymph nodes or parasites could restrict the flow of lymph fluid. Infection-associated lymphedema is most frequent in tropical and subtropical regions and is more likely to happen in developing countries.
CAUSES OF PRIMARY LYMPHEDEMA
Primary lymphedema is an uncommon, inherited condition caused by problems with the development of lymph vessels in your body. Certain causes of primary lymphedema include:
- Milroy’s disease (congenital lymphedema) – This disorder starts in infancy and causes lymph nodes to form abnormally.
- Meige’s disease (lymphedema praecox) – This disorder generally causes lymphedema around puberty or during pregnancy, though it could happen later, until age 35.
- Late-onset lymphedema (lymphedema tarda) – This happens rarely and generally starts after age 35.
neuroendoscopy
LYMPHEDEMA RISK FACTORS
Factors that might increase your risk of developing lymphedema after cancer, from cancer treatment, or from other secondary causes include:
- Older age
- Excess weight or obesity
- Rheumatoid or psoriatic arthritis
LYMPHEDEMA COMPLICATIONS
Lymphedema in your arm or leg could lead to severe complications, such as:
- Infections – Possible infections that could result from lymphedema include a severe bacterial infection of the skin (cellulitis) and an infection of the lymph vessels (lymphangitis). The smallest injury to your arm or leg could be an entry point for infection.
- Lymphangiosarcoma – This uncommon form of soft tissue cancer could result from the most serious cases of untreated lymphedema. Potential signs of lymphangiosarcoma include blue-red or purple marks on the skin.
LYMPHEDEMA PREVENTION
If you have had or you are going to have cancer surgery, ask your doctor or primary care physician whether your procedure will involve your lymph nodes or lymph vessels. Ask if your radiation treatment will be aimed at lymph nodes, so you will be aware of the possible risks.
To lower your risk of lymphedema, try to:
- Protect your arm or leg – Avoid injury to your damaged limb. Cuts, scrapes, and burns could invite infection. Protect yourself from pointed objects. For instance, shave with an electric razor, wear gloves when you garden or cook, and use a thimble when you sew. If possible, avoid medical procedures, like blood draws and vaccinations, in your damaged limb.
- Rest your arm or leg while recovering – After cancer treatment is complete, exercise and stretching are encouraged. But circumvent strenuous activity until you have recovered from surgery or radiation.
- Avoid heat on your arm or leg – Do not apply ice or heat, like with a heating pad, to your damaged limb. Also, protect your damaged limb from extreme cold.
- Elevate your arm or leg – Whenever possible, elevate your damaged limb above the level of your heart.
- Avoid tight clothing – Avoid anything that could constrict your arm or leg, like tightfitting clothing and, in the case of your arm, blood pressure cuffs. Request that your blood pressure be taken in your other arm.
- Keep your arm or leg clean – Make skincare and nail care high priorities. Inspect the skin on your arm or leg daily, watching for changes or breaks in your skin that can lead to infection. Do not go barefoot.
LYMPHEDEMA DIAGNOSIS
If you are at risk of lymphedema for example if you have recently had cancer surgery including your lymph nodes your doctor or primary care physician might diagnose lymphedema based upon your signs and symptoms.
If the cause of your lymphedema is not so clear, your doctor or primary care physician might order imaging tests to check your lymph system. Tests might include:
- Magnetic Resonance Imaging (MRI) scan – Using a magnetic field and radio waves, magnetic resonance imaging (MRI) produces 3-D, high-resolution images.
- Computed Tomography (CT) scan – This X-ray technique produces detailed, cross-sectional images of your body’s structures. Computed Tomography (CT) scans could reveal blockages in the lymphatic system.
- Doppler ultrasound – This form of conventional ultrasound looks at blood flow and pressure by bouncing high-frequency sound waves (ultrasound) off red blood cells. Ultrasound could help find obstructions.
- Radionuclide imaging of your lymphatic system (lymphoscintigraphy) – At the time of this test, you will be administered with a radioactive dye and then scanned by a machine. The resulting pictures show the dye moving through your lymph vessels, highlighting obstructions.
LYMPHEDEMA TREATMENT
There is no cure for lymphedema. Treatment focuses on reducing inflammation and controlling the pain. Lymphedema treatments include:
- Exercises – Light or easy exercises in which you move your damaged body part or limb might improve lymph fluid flow and help prepare you for everyday activities, for example carrying groceries. Exercises should not be strenuous or exhaust you but should focus on gentle contraction of the muscles in your arm or leg. A certified lymphedema therapist could teach you exercises that might help.
- Bandaging your arm or leg – Dressing your complete limb assists lymph liquid to flow back toward the trunk of your body. The bandage must be tight around your fingers or toes and loosen as it moves up your arm or leg. A lymphedema therapist could show you how to wrap your limb.
- Massage – A special massage technique known as manual lymph drainage might encourage the flow of lymph fluid out of your arm or leg. And various massage treatments might benefit people with active cancer. Make sure to work with someone who is specially trained in these techniques. Massage is not for everyone. Avoid or circumvent massage if you have a skin infection, blood clots, or an active illness or disease in the involved lymph drainage regions.
- Pneumatic compression – A sleeve worn over your damaged arm or leg joins to a pump that sometimes inflates the sleeve, putting pressure on your limb and moving lymph liquid away from your fingers or toes.
- Compression garments – Lengthy sleeves or stockings designed to compress your arm or leg improve the flow of the lymph liquid out of your damaged body part or limb. Wear a compression garment during the workout of the damaged body part or limb. Get the correct fit for your compression garment by getting professional assistance. Ask your doctor or primary care physician where you could buy compression garments in your community. Some people will need custom-made compression garments. If you have trouble putting on or taking off the compression garment, there are special techniques or methods and aids to help with this your lymphedema therapist could check alternatives with you. Additionally, if compression garments or compression wraps, or both aren’t an alternative, at times a compression device with fabric fasteners could work for you.
- Complete decongestive therapy (CDT) – Complete decongestive therapy (CDT) approach includes combining therapies with lifestyle alterations. In most cases, complete decongestive therapy (CDT) is not suggested for people or individuals who have high blood pressure, diabetes, paralysis, heart failure, blood clots, or acute infections.
In cases of serious lymphedema, your doctor or primary care physician might consider surgery to remove excess tissue in your arm or leg to lower inflammation. There are also new methods or techniques for surgery that may be correct, like lymphatic to venous anastomosis or lymph node transplants.
If you or anyone you know is suffering from lymphedema, our expert providers at Specialty Care Clinics will take care of your health and help you recover.
Call 469-545-9983 to book a telehealth appointment for an at-home check-up.
