WHAT IS BEHCET’S DISEASE?
Behcet’s disease, also known as Behcet’s syndrome, is an uncommon disorder that causes blood vessel inflammation throughout your body.
The disease could lead to numerous signs and symptoms that could seem unrelated at first. They could include mouth sores, eye swelling, skin rashes and lesions, and genital sores.
Treatment involves medications to lower the signs and symptoms of Behcet’s disease and to prevent serious complications, like blindness.
BEHCET’S DISEASE SYMPTOMS
Behcet’s disease symptoms vary from person to person, could come and go or become less serious over time. Signs and symptoms depend upon which parts of your body are affected.
Areas frequently affected by Behcet’s disease include:
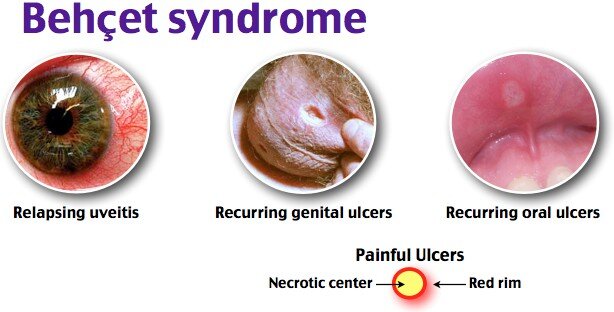
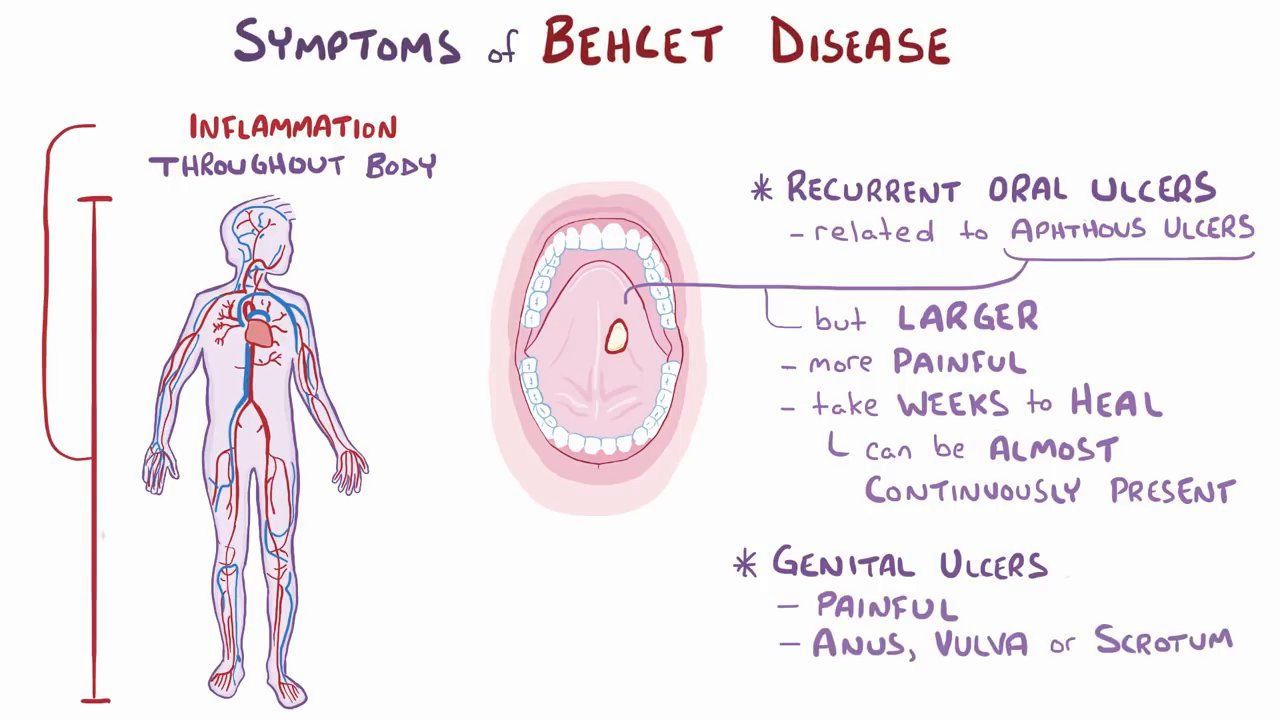
- Mouth – Painful mouth sores that look similar to canker sores are the most frequent sign of Behcet’s disease. They start as raised, round lesions in the mouth that quickly turn into painful ulcers. The sores generally heal in 1 to 3 weeks, though they do recur.
- Skin – Some people develop acne identical to sores on their bodies. Others develop red, raised, and tender nodules on their skin, generally on the lower legs.
- Genitals – Red, open sores could happen on the scrotum or the vulva. The sores are generally painful and could leave scars.
- Eyes – Inflammation in the eye (uveitis) causes redness, pain, and blurred vision, generally in both eyes. In people with Behcet’s disease, the condition could come and go.
- Joints – Joint inflammation and pain usually affect the knees in people with Behcet’s disease. The ankles, elbows, or wrists also may be involved. Signs and symptoms could last 1 to 3 weeks and go away on their own.
- Blood vessels – Swelling in veins and arteries could cause redness, pain, and swelling in the arms or legs when a blood clot results. Swelling in the large arteries could lead to complications, like aneurysms and narrowing or blockage of the vessel.
- Digestive system – A variety of signs and symptoms could affect the digestive system, including abdominal pain, diarrhea, and bleeding.
- Brain – Inflammation in the brain and nervous system could cause headaches, fever, disorientation, poor balance, or stroke.
WHEN SHOULD YOU SEE A DOCTOR?
Make an appointment with your doctor or primary care physician if you notice unusual signs and symptoms that may indicate Behcet’s disease. If you have been diagnosed with the condition, see your doctor or primary care physician if you notice new signs and symptoms.

BEHCET’S DISEASE CAUSES
Behcet’s disease may be an autoimmune disorder, which means the body’s immune system mistakenly attacks some of its own healthy cells. It is likely that genetic and environmental factors play a role.
The signs and symptoms of Behcet’s disease are considered to be because of inflammation of the blood vessels (vasculitis). The condition could involve arteries and veins of all sizes, damaging them throughout the body.
Several genes have been found to be related to the disease. Some researchers believe a virus or bacterium could trigger Behcet’s disease in people who have specific genes that make them vulnerable to Behcet’s.
BEHCET’S DISEASE RISK FACTORS
Factors that may increase your risk of Behcet’s disease include:
- Age – Behcet’s disease frequently affects men and women in their 20s and 30s, though children and older adults also could develop the condition.
- Where you live – People from countries in the Middle East and East Asia, including Turkey, Iran, Japan, and China, are more likely to develop Behcet’s disease.
- Sex – While Behcet’s disease happens in both men and women, the disease is generally more serious in men.
- Genes – Having specific genes is related to a higher risk of developing Behcet’s.
BEHCET’S DISEASE COMPLICATIONS
Complications of Behcet’s disease depend upon your signs and symptoms. For example, untreated uveitis could lead to decreased vision or blindness. People with eye signs and symptoms of Behcet’s disease require to visit an eye specialist (ophthalmologist) regularly because treatment could help prevent this complication.
BEHCET’S DISEASE DIAGNOSIS
No tests could determine whether you have Behcet’s disease, so your doctor or primary care physician will rely mainly on your signs and symptoms. Because nearly everyone with the condition develops mouth sores, mouth sores that have recurred at least 3 times in twelve months are usually required for a diagnosis of Behcet’s disease.
In addition, a diagnosis of Behcet’s disease needs at least two additional signs, like:
- Recurring genital sores
- Eye inflammation
- Skin sores
Tests you may require include:
- Blood tests or other lab tests may rule out other conditions.
- Pathergy test, in which your doctor or primary care physician inserts a sterile syringe into your skin and examines the region one to two days later. If the test is positive, a small red bump forms under your skin where the syringe was inserted. This indicates your immune system is overreacting to a minor injury.
BEHCET’S DISEASE TREATMENT
There is no cure for Behcet’s disease. If you have a mild form, your doctor or primary care physician may recommend medications to control the pain and inflammation of flares. You may not require medication between flares.
For more serious signs and symptoms, your doctor or primary care physician may prescribe medications to control Behcet’s disease throughout your body, in addition to medications for flares.
Treatments for specific signs and symptoms of Behcet’s disease
Medications to control signs and symptoms you have during flares may include the following:
Skin creams, gels, and ointments – Topical corticosteroid medicines are applied directly to skin and genital sores to lower swelling and pain.
Mouth rinses – Using special mouthwashes that contain corticosteroids and other agents may lower the pain of mouth sores.
Eye drops – Eye drops containing corticosteroids or other anti-inflammatory medicines could relieve pain and redness in your eyes if swelling is mild.
Systemic treatments for Behcet’s disease
If topical medications do not help, your doctor or primary care physician may suggest a drug known as colchicine (Colcrys, Mitigare) for recurring oral and genital sores. Joint inflammation also may improve with colchicine.
Serious cases of Behcet’s disease need treatments to control damage from the disease between flares. If you have moderate to severe Behcet’s disease, your doctor or primary care physician may prescribe:
Corticosteroids to control inflammation – Corticosteroids, like prednisone, are used to lower the swelling caused by Behcet’s disease. Doctors or primary care physicians usually prescribe them another medication to suppress the activity of their immune system.
Side effects of corticosteroids include weight gain, continuous heartburn, high blood pressure, and bone thinning (osteoporosis).
Medications that suppress your immune system – The swelling related to Behcet’s disease could be lowered by drugs that prevent your immune system from attacking healthy tissues. These drugs might include azathioprine (Azasan, Imuran), cyclosporine (Gengraf, Neoral, Sandimmune), and cyclophosphamide. These drugs could increase your risk of infection. Other possible side effects include liver and kidney issues, low blood counts, and high blood pressure.
Medications that alter your immune system’s response – Interferon alfa-2b (Intron A) regulates the activity of your immune system to control swelling. It might be used alone or with other drugs to help control skin sores, joint pain, and eye swelling in people with Behcet’s disease. Side effects include flu-like signs and symptoms, like muscle pain and fatigue.
Medications that block a substance known as tumor necrosis factor (TNF) are effective in treating some of the signs and symptoms of Behcet’s, particularly for people who have more serious or resistant symptoms. Instances include infliximab (Remicade) and adalimumab (Humira). Side effects may include headaches, skin rash, and an increased risk of infections.
If you or anyone you know is suffering from Behcet’s disease, our expert providers at Specialty Care Clinics will take care of your health and help you recover.
Call 469-545-9983 to book a telehealth appointment for an at-home check-up.
