WHAT IS UTERINE PROLAPSE?
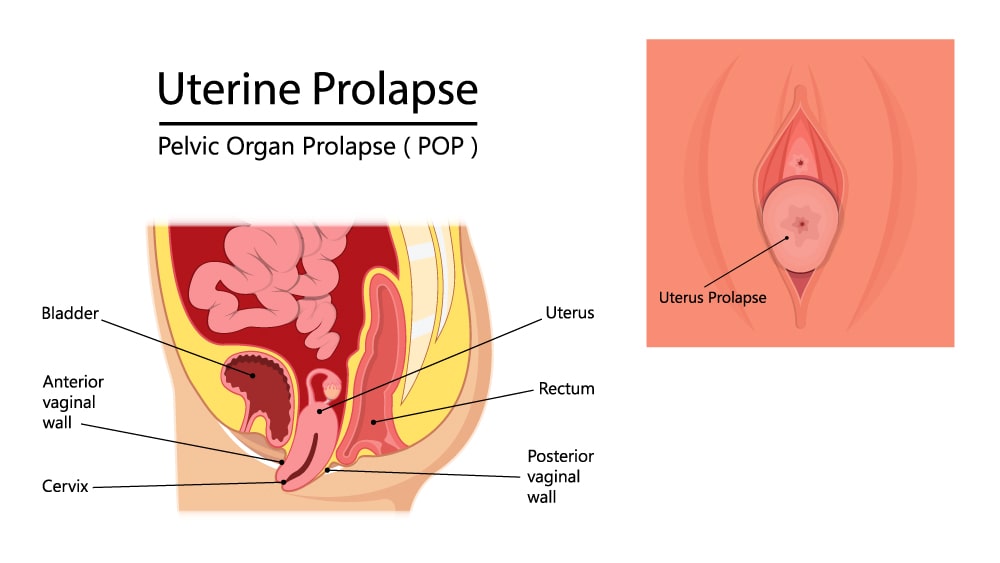
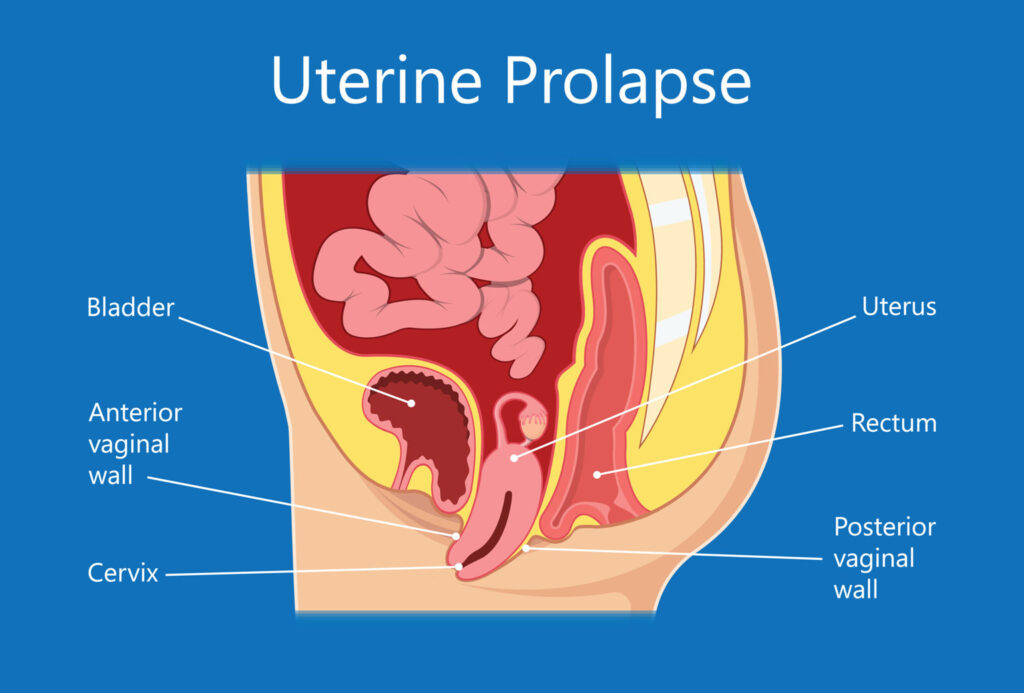
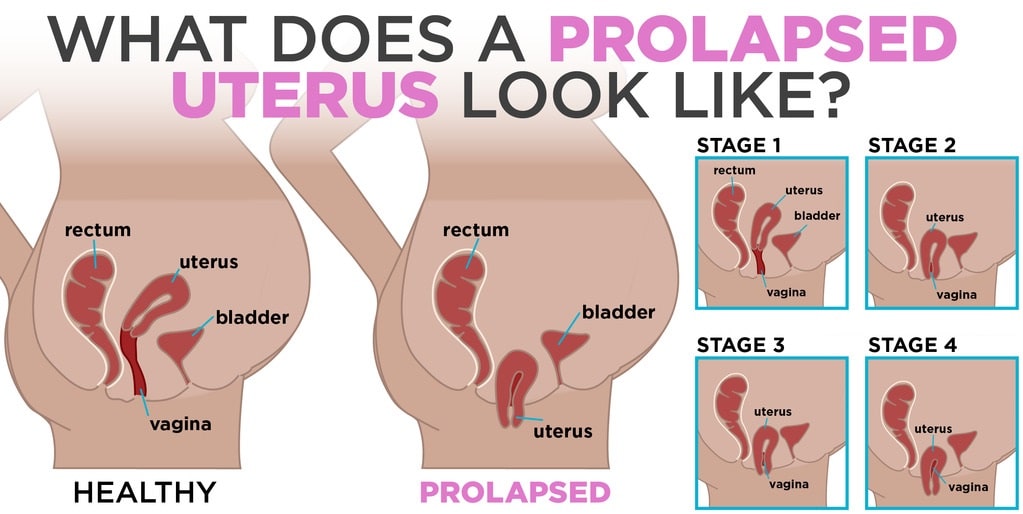
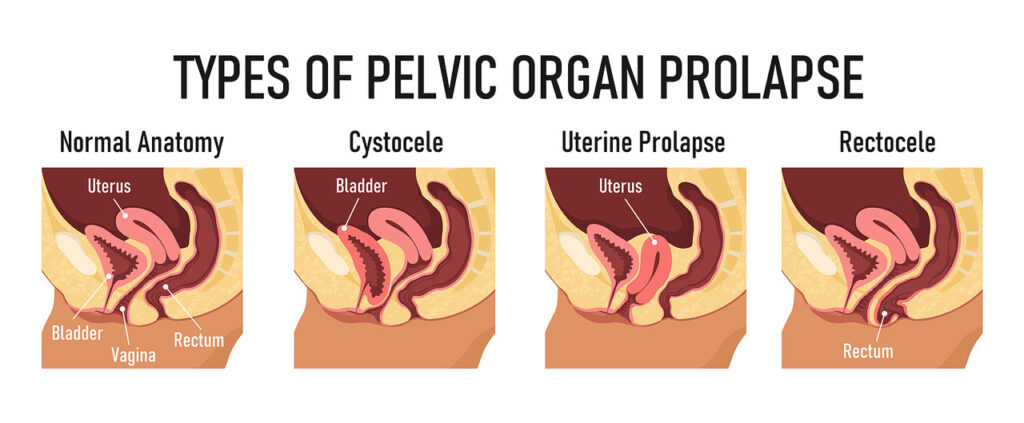
Uterine prolapse happens when pelvic floor muscles and ligaments stretch and weaken and no longer offer enough support for the uterus. As a consequence, the uterus slips down into or protrudes out of the vagina.
Uterine prolapse could occur in women of any age. But it usually affects postmenopausal women who have had one or more vaginal deliveries.
Mild uterine prolapse generally does not require treatment. But if uterine prolapse makes you uncomfortable or disturbs your normal life, you may benefit from treatment.
UTERINE PROLAPSE SYMPTOMS
Mild uterine prolapse usually does not cause signs or symptoms. Signs and symptoms of moderate to severe uterine prolapse are as follows:
- Feeling of heaviness or pulling within your pelvis.
- Tissue bulging from your vagina.
- Urinary problems, like urine leakage (incontinence) or urine retention.
- Difficulty having a bowel movement.
- Feeling like you are sitting on a small ball or as if something is falling out of your vagina.
- Sexual concerns, like a feeling of looseness in the tone of your vaginal tissue.
Usually, symptoms are less bothersome in the morning and get worse as the day goes on.
WHEN SHOULD YOU SEE A DOCTOR?
Consult your doctor to talk about your options if signs and symptoms of uterine prolapse become bothersome and disturb your normal activities.
UTERINE PROLAPSE CAUSES
Uterine prolapse develops from the weakening of pelvic muscles and supportive tissues. Causes of weakened pelvic muscles and tissues are as follows:
- Pregnancy.
- Difficult labor and childbirth or trauma during delivery.
- Delivery of a large baby.
- Being overweight or obese.
- Lower estrogen level after menopause.
- Chronic constipation or straining with bowel movements.
- Chronic cough or bronchitis.
- Repeated heavy lifting.
UTERINE PROLAPSE RISK FACTORS
Factors that could increase your risk of uterine prolapse include:
- One or more pregnancies and vaginal births.
- Giving birth to a big baby.
- Increasing age.
- Obesity.
- Prior pelvic surgery.
- Chronic constipation or frequent exertion during bowel movements.
- Family history of weakness in connective tissue.
- Being Hispanic or white.
UTERINE PROLAPSE COMPLICATIONS
Uterine prolapse is usually related to the prolapse of other pelvic organs. You may experience:
- Anterior prolapse (cystocele) – Weakness of connective tissue separating the bladder and vagina might cause the bladder to protrude into the vagina. Anterior prolapse is also known as the prolapsed bladder.
- Posterior vaginal prolapse (rectocele) – Weakness of connective tissue separating the rectum and vagina might cause the rectum to protrude into the vagina. You may have trouble having bowel movements.
Severe uterine prolapse could displace part of the vaginal lining, causing it to protrude outside the body. Vaginal tissue that rubs against clothing could lead to vaginal sores (ulcers.) Sometimes, the sores could become infected.
UTERINE PROLAPSE PREVENTION
To lower your risk of uterine prolapse, try to:
- Perform Kegel exercises regularly – These exercises could strengthen your pelvic floor muscles — particularly important after you have a baby.
- Treat and prevent constipation – Drink plenty of fluids and eat high-fiber foods, like fruits, vegetables, beans, and whole-grain cereals.
- Avoid heavy lifting and lift correctly – When lifting, use your legs in place of your waist or back.
- Control coughing – Get treatment for a chronic cough or bronchitis, and do not smoke.
- Avoid weight gain – Speak with your doctor to determine your ideal weight and get advice on weight-loss strategies, if you require them.
UTERINE PROLAPSE DIAGNOSIS
A diagnosis of uterine prolapse usually happens during a pelvic examination.
During the pelvic examination your doctor will probably ask you:
- To bear down like having a bowel movement. Bearing down could help your doctor assess how far the uterus has slipped into the vagina.
- To tighten your pelvic muscles as if you are preventing a stream of urine. This test examines the strength of your pelvic muscles.
You may fill out a questionnaire that helps your doctor evaluate how uterine prolapse affects your quality of life. This information helps direct treatment decisions.
If you have severe incontinence, your doctor may suggest tests to measure how well your bladder functions (urodynamic testing).

UTERINE PROLAPSE TREATMENT
Treatment depends upon the severity of uterine prolapse. Your doctor may recommend:
- Self-care measures – If your uterine prolapse causes few or no symptoms, simple self-care measures might provide relief or help prevent worsening prolapse. Self-care measures involve doing Kegel exercises to strengthen your pelvic muscles, losing weight, and treating constipation.
- Pessary – A vaginal pessary is a plastic or rubber ring inserted into your vagina to support the protruding tissues. A pessary should be removed regularly for cleaning.
UTERINE PROLAPSE SURGERY
Your doctor may recommend surgery to repair uterine prolapse. Minimally invasive (laparoscopic) or vaginal surgery may be an option.
Surgery could involve:
- Repair of weakened pelvic floor tissues – This surgery is usually approached through the vagina but sometimes through the abdomen. The surgeon may graft your own tissue, donor tissue, or a synthetic material onto weakened pelvic floor structures to support your pelvic organs.
- Removal of your uterus (hysterectomy) – Hysterectomy may be recommended for uterine prolapse in specific instances. A hysterectomy is usually very safe, but with any surgery comes the risk of complications.
Speak with your doctor about all your treatment options to be sure you understand the risks and benefits of each so that you could choose what is best for you.
If you or anyone you know is suffering from uterine prolapse, our expert providers at Specialty Care Clinics will take care of your health and help you recover.
Call 469-545-9983 to book a telehealth appointment for an at-home check-up.
