ABDOMINAL AORTIC ANEURYSM – SYMPTOMS, CAUSES, AND TREATMENT
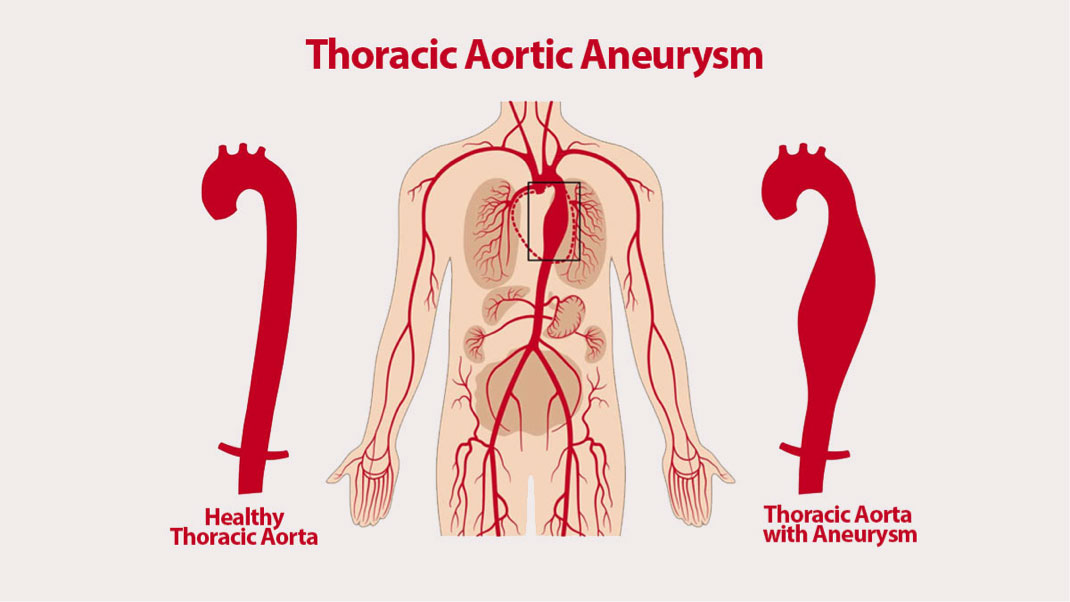
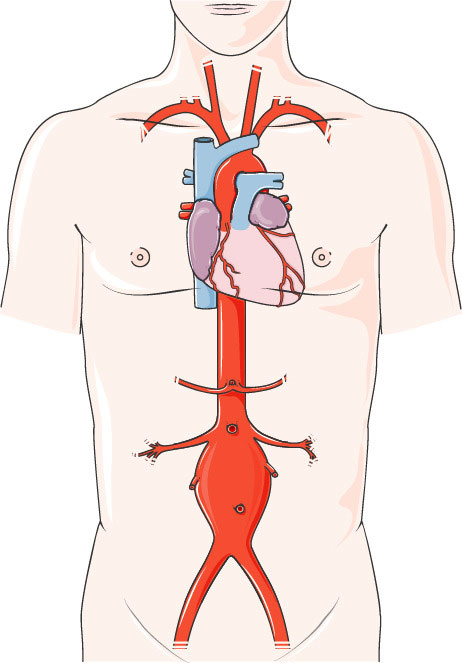
An abdominal aortic aneurysm (AAA) is a swollen region in the lower part of the important vessel that supplies blood to the body (aorta). The aorta runs from your heart through the center of your chest and stomach.
The aorta is the biggest blood vessel in the body, so a ruptured abdominal aortic aneurysm could cause life-threatening bleeding.
Depending upon the size of the aneurysm and how fast it is growing, treatment varies from watchful waiting to emergency surgery.
ABDOMINAL AORTIC ANEURYSM SYMPTOMS
Abdominal aortic aneurysms usually grow gradually without symptoms, making them hard to detect. There are aneurysms that never rupture. Many start small and stay small others expand over time, some rapidly.
If you have an enlarging abdominal aortic aneurysm, you may notice:
- Deep, continuous pain in your abdomen or on the side of your abdomen
- Back pain
- A pulse near your bellybutton
WHEN SHOULD YOU SEE A DOCTOR?
If you have pain, particularly if the pain is unexpected and serious, look for immediate medical help.
ABDOMINAL AORTIC ANEURYSM CAUSES
Aneurysms could develop anywhere along the aorta, but most aortic aneurysms happen in the part of your aorta that is in your abdomen. A number of factors could play a role in developing an aortic aneurysm, including:
- Hardening of the arteries (atherosclerosis) – Atherosclerosis happens when fat and other substances accumulate on the lining of a blood vessel.
- High blood pressure – High blood pressure could damage and weaken the aorta’s walls.
- Blood vessel diseases – These are diseases that cause blood vessels to become swollen.
- Infection in the aorta – Rarely, a bacterial or fungal infection may cause abdominal aortic aneurysms.
- Trauma – For instance, being in a car accident could cause abdominal aortic aneurysms
ABDOMINAL AORTIC ANEURYSM RISK FACTORS
Abdominal aortic aneurysm risk factors include:
- Tobacco use – Smoking is the primary risk factor. It could weaken the aortic walls, raising the risk not only of developing an aortic aneurysm but of rupture. The more and more you smoke or chew tobacco, the higher the chances of developing an aortic aneurysm.
- Age – These aneurysms happen most usually in people age 65 years and older.
- Being male – Men develop abdominal aortic aneurysms much more usually than women do.
- Being white – People who are white are at greater risk of abdominal aortic aneurysms.
- Family history – Having a family history of abdominal aortic aneurysms raises your risk of developing the disease.
- Other aneurysms – Having an aneurysm in another big blood vessel, like the artery behind the knee or the aorta in the chest, may raise your risk of an abdominal aortic aneurysm.
ABDOMINAL AORTIC ANEURYSM COMPLICATIONS
Tears in one or more of the layers of the wall of the aorta (aortic dissection) or a ruptured aneurysm are the primary complications. A rupture could cause life-threatening internal bleeding. In general, the bigger the aneurysm and the faster it grows, the higher the risk of rupture.
Signs and symptoms that your aortic aneurysm has ruptured could include:
- Unexpected, intense, and persistent abdominal or back pain, which could be described as a tearing sensation
- Low blood pressure
- Fast pulse
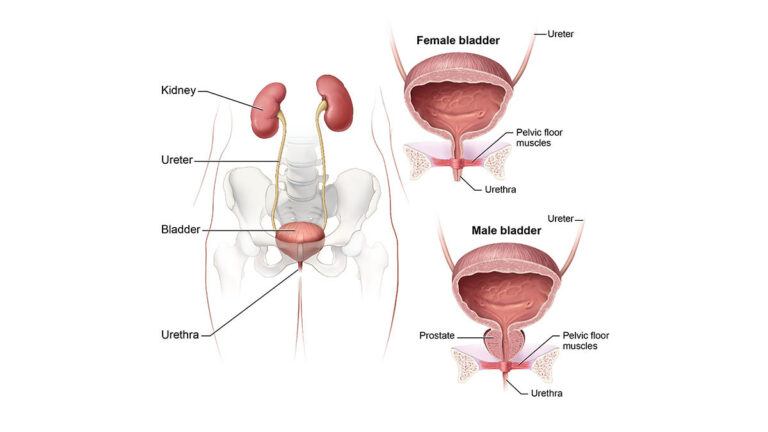
Aortic aneurysms also put you at risk of developing blood clots in the region. If a blood clot breaks loose from the inside wall of an aneurysm and obstructs a blood vessel elsewhere in your body, it could cause pain or block the blood circulation to the legs, toes, kidneys, or abdominal organs.
ABDOMINAL AORTIC ANEURYSM PREVENTION
To prevent an aortic aneurysm or keep an aortic aneurysm from getting worse, do the following:
- Do not use tobacco products – Quit smoking or chewing tobacco and circumvent secondhand smoke.
- Eat a healthy diet – Concentrate on eating a variety of fruits and vegetables, whole grains, poultry, fish, and low-fat dairy products. Circumvent saturated fat, trans fats, and limit salt.
- Keep your blood pressure and cholesterol under control – If your doctor or primary care physician has prescribed medications, take them as instructed.
- Get regular exercise – Try to get at least 150 minutes per week of moderate aerobic activity. If you have not been active, start gradually and build up. Talk to your doctor or primary care physician about what kinds of activities are right for you.
If you are at risk of an aortic aneurysm, your doctor or primary care physician may suggest other measures, like medications to lower your blood pressure and relieve stress on weakened arteries.
ABDOMINAL AORTIC ANEURYSM DIAGNOSIS
Abdominal aortic aneurysms are usually found during an examination for another reason or during routine medical tests, like an ultrasound of the heart or abdomen.
To diagnose an abdominal aortic aneurysm, doctors or primary care physicians will review your medical and family history and do a physical examination. If your doctor or primary care physician suspects that you have an aortic aneurysm, specialized tests, like the following, could confirm it.
- Abdominal ultrasound – This test is most frequently used to diagnose abdominal aortic aneurysms. You lie down on a table while a technician moves a wand (transducer) around your abdomen. Ultrasound uses sound waves to send pictures to a computer screen.
- Computerized Tomography (CT) scan – This painless test could provide your doctor or primary care physician with clear pictures of your aorta, and it could detect the size and shape of an aneurysm. During a computerized tomography (CT) scan, you lie down on a table inside a doughnut-shaped machine. Computerized Tomography (CT) scanning generates X-rays to produce cross-sectional pictures of your body. You may have contrast dye administered into your blood vessels that make your arteries more visible on the computerized tomography (CT) pictures (CT angiography).
- Magnetic Resonance Imaging (MRI) – In this test, you lie down on a movable table that slides into a machine. Magnetic resonance imaging (MRI) uses a magnetic field and pulses of radio wave energy to make images of your body. You may have a dye administered into your blood vessels to make them more visible (magnetic resonance angiography).
Abdominal Aortic Aneurysm Screening
Being male and smoking significantly raises the risk of abdominal aortic aneurysms. Screening recommendations vary, but generally:
- Men ages 65 to 75 years who have ever smoked cigarettes should have a one-time screening using abdominal ultrasound.
- For men ages, 65 to 75 years who have never smoked, your doctor or primary care physician will decide on the need for an abdominal ultrasound, generally based on other risk factors, like a family history of aneurysm.
There is not enough evidence to determine whether women ages 65 to 75 years who ever smoked cigarettes or have a family history of an abdominal aortic aneurysm would benefit from abdominal aortic aneurysm screening. Ask your doctor or primary care physician if you need to have an ultrasound screening based on your risk factors. Women who have never smoked generally do not need to be screened for the condition.
ABDOMINAL AORTIC ANEURYSM TREATMENT
The objective of treatment either medical monitoring or surgery is to stop your aneurysm from rupturing. Which treatment you have depends upon the size of the aortic aneurysm and how fast it is developing.
Medical monitoring
Your doctor or primary care physician may recommend this option if your abdominal aortic aneurysm is small and you do not have symptoms. You will have regular appointments to check if your aneurysm is growing, and treatment to manage other medical conditions, like high blood pressure, that could worsen your aneurysm.
It is likely you will need regular imaging tests to check on the size of your aneurysm. Expect to have an abdominal ultrasound at least six months after your aneurysm is diagnosed and at regular follow-up examinations.
Abdominal Aortic Aneurysm Surgery
Repair is usually suggested if your aneurysm is 1.9 to 2.2 inches (4.8 to 5.6 centimeters) or bigger or if it is growing rapidly. In addition to this, your doctor or primary care physician may suggest surgery if you have symptoms like abdominal pain or you have a leaking, tender or painful aneurysm.
Depending on various factors, including location and size of the aneurysm, your age, and other conditions you have, repair options may include:
Open abdominal surgery – The aim is to remove the affected portion of the aorta and replacing it with a synthetic tube (graft), which is stitched in place. It will probably take a month or more to complete recovery.
Endovascular repair – This less invasive procedure is used more usually. Doctors or primary care physicians attach a synthetic graft to the end of a thin tube (catheter) that is inserted through an artery in your leg and threaded within your aorta. The graft — a woven tube covered by a metal mesh support — is implanted at the site of the aneurysm, expanded, and fastened in place. It strengthens the weakened section of the aorta to stop the rupture of the aneurysm. Endovascular surgery is not an option for about thirty percent of people with an aneurysm. After endovascular surgery, you will require regular imaging tests to make sure that the repair is not leaking.
Long-term survival rates are the same for both endovascular surgery and open surgery.
If you or anyone you know is suffering from an abdominal aortic aneurysm, our expert providers at Specialty Care Clinics will take care of your health and help you recover.
Call (469) 545-9983 to book an appointment for an at-home check-up.
