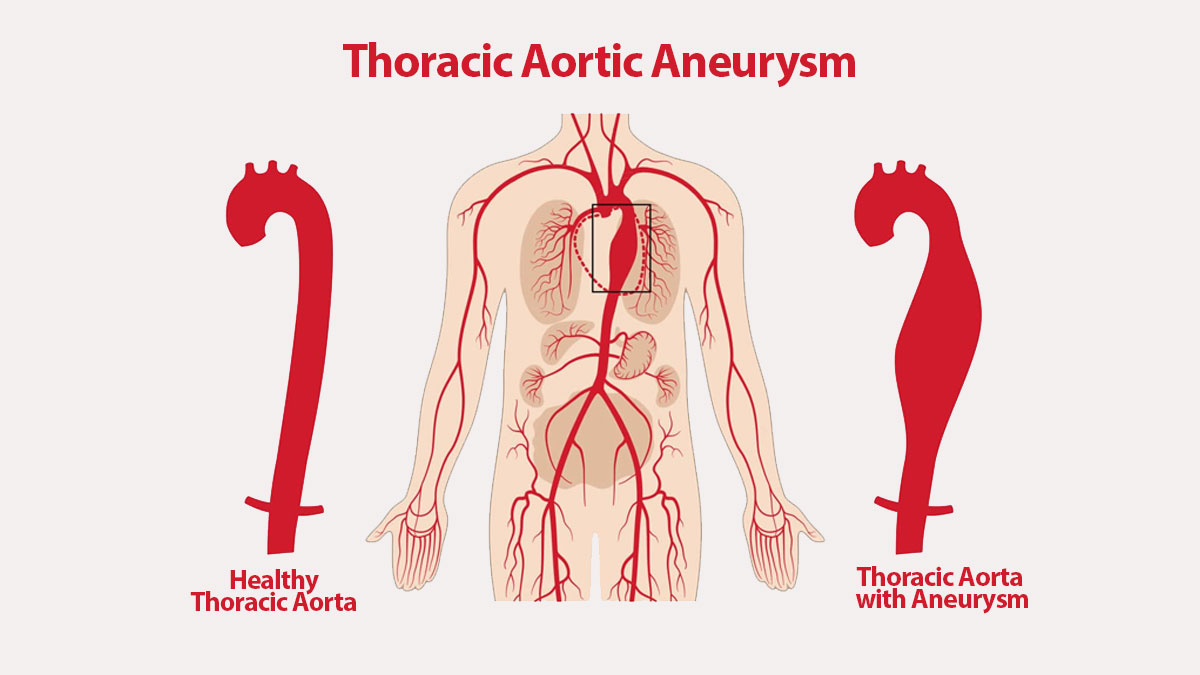
WHAT IS A THORACIC AORTIC ANEURYSM?
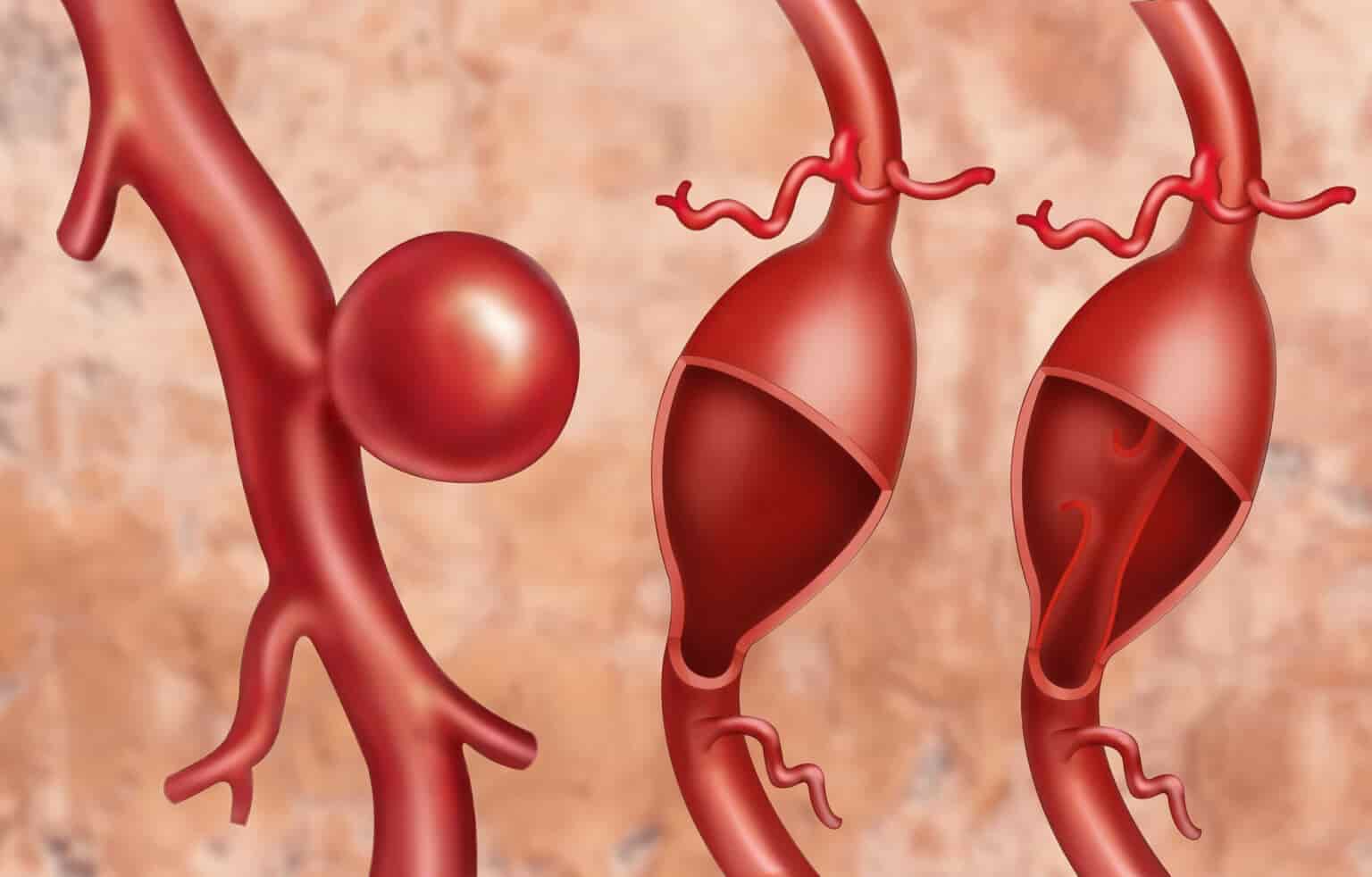
A thoracic aortic aneurysm is a weakened region in the major blood vessel that feeds blood to the body (aorta). When the aorta is weak, blood pushing against the vessel wall could cause it to protrude like a balloon (aneurysm).
A thoracic aortic aneurysm is also known as a thoracic aneurysm, and aortic dissection could happen because of an aneurysm. A dissection is a tear in the wall of the aorta that could cause life-threatening bleeding or unexpected death. Large, fast-growing aneurysms also might rupture, but small and slow-growing aneurysms might never rupture.
Depending on the cause, size, and growth rate of your thoracic aortic aneurysm, treatment might vary from watchful waiting to emergency surgery. Ideally, surgery could be planned if necessary.
THORACIC AORTIC ANEURYSM SYMPTOMS
Thoracic aortic aneurysms often grow gradually and generally without symptoms, making them difficult to detect. There are aneurysms that never rupture. Many start small and stay small, however some expand over time. How quickly an aortic aneurysm might grow is difficult to predict.
As a thoracic aortic aneurysm grows, some people might notice:
- Tenderness or pain in the chest
- Back pain
- Hoarseness
- Cough
- Shortness of breath
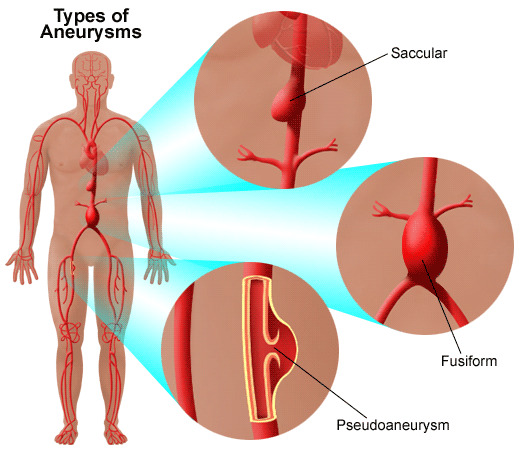
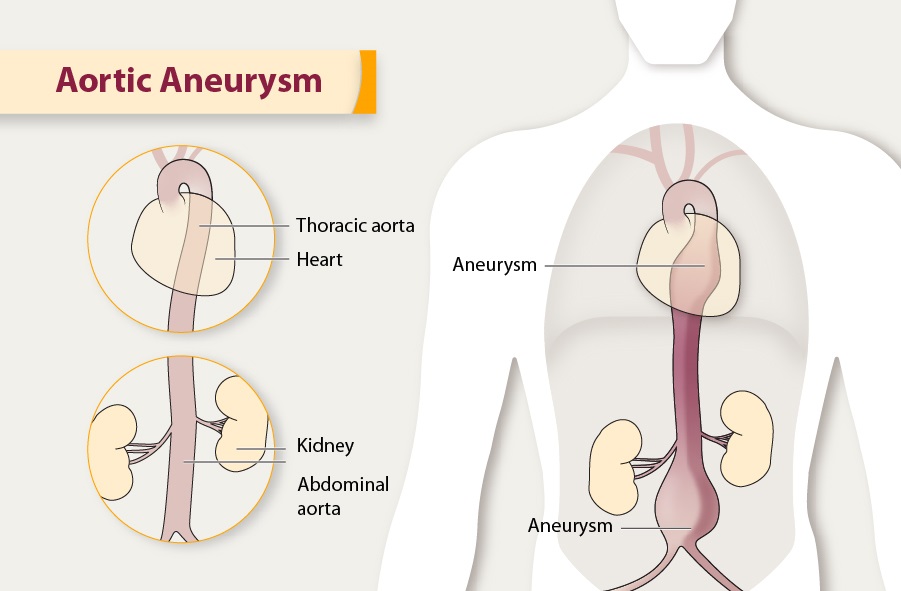
Aortic aneurysms could develop anywhere along the aorta, which runs from your heart through your chest and abdomen. When they happen in the chest, they are known as thoracic aortic aneurysms. Aneurysms could happen anywhere in the thoracic aorta, including near the heart, in the aortic arch, and in the lower part of the thoracic aorta.
Thoracic aortic aneurysms are less frequent than aneurysms that form in the lower part of your aorta (abdominal aortic aneurysms). An aneurysm could also happen in between the upper and lower parts of your aorta. This type of aneurysm is known as a thoracoabdominal aneurysm.
WHEN SHOULD YOU SEE A DOCTOR?
Most people with aortic aneurysms do not have symptoms unless a tear or rupture happens. A dissection or burst is a medical emergency. Call 911 or your local emergency number if you need immediate help.
If an aneurysm ruptures or one or more layers of the artery wall tears, you might feel:
- Sharp, unexpected pain in the upper back that radiates downward
- Pain in your chest, jaw, neck, and arms
- Trouble breathing
If you have a family history of aortic aneurysm, Marfan syndrome or another connective tissue disease (CTD), or a bicuspid aortic valve, your doctor or primary care physician might recommend regular ultrasound or radiology testing like CT scans or MRI exams to screen for aortic aneurysm.
THORACIC AORTIC ANEURYSM CAUSES
Factors that could contribute to an aneurysm’s development include:
- Hardening of the arteries (atherosclerosis) – As plaque accumulates on your artery walls, they become less flexible, and the additional pressure could cause them to weaken and protrude. High blood pressure and high cholesterol are risk factors for solidifying the arteries. This is more frequent in senior citizens.
- Genetic conditions – Aortic aneurysms in younger people usually have a genetic cause. People who are born with Marfan syndrome, a genetic condition that affects the connective tissue in the body, are especially at risk of a thoracic aortic aneurysm because they might have weakness in the aortic wall.
Marfan syndrome usually causes distinct physical traits, including tall stature, very long arms, a deformed breastbone, and eye issues.
Other family-associated disorders could cause an aortic aneurysm, including vascular Ehlers-Danlos, Loeys-Dietz, and Turner syndromes. Vascular Ehlers-Danlos syndrome causes your skin, joints, and connective tissue to be delicate and makes your skin stretch easily. - Other medical conditions – Inflammatory conditions, like giant cell arteritis and Takayasu arteritis, are related to thoracic aortic aneurysms.
- Problems with your heart’s aortic valve – Sometimes people who have issues with the valve that blood flows through as it leaves the heart (aortic valve) have an increased risk of thoracic aortic aneurysm. This is primarily true for people who were born with an aortic valve that has only two flaps instead of three (bicuspid aortic valve).
- Untreated infection – Though rare, it is possible to develop a thoracic aortic aneurysm if you have had an untreated infection, like syphilis or salmonella.
- Traumatic injury – Rarely, some people who are injured in falls or car accidents develop thoracic aortic aneurysms.
Aortic emergencies
In aortic dissection, a tear happens within the wall of the aorta. This causes bleeding into and along the aortic wall and, in some cases, entirely out of the aorta (rupture).
An aortic dissection is a possible life-threatening emergency, depending on where in the aorta it happens. It is crucial to treat an aortic aneurysm to try to prevent dissection. If dissection happens, people could still be treated with surgery, but they will have a higher risk of complications.
THORACIC AORTIC ANEURYSM RISK FACTORS
Thoracic aortic aneurysm risk factors include:
- Age – Thoracic aortic aneurysms happen most usually in people age 65 years and older.
- Tobacco use – Tobacco use is a major risk factor for the development of an aortic aneurysm.
- High blood pressure – Increased blood pressure damages the blood vessels in the body, increasing your chances of developing an aneurysm.
- The build-up of plaques in your arteries – The accumulation of fat and other substances that could damage the lining of a blood vessel increases your risk of an aneurysm. This is a more common risk in senior citizens.
- Family history – People who have a family history of aortic aneurysm are at increased risk of developing one. A family history means you might develop aneurysms at a younger age and you are at higher risk of rupture. This is the main risk factor in younger people.
- Marfan syndrome and associated conditions – If you have Marfan syndrome or an associated condition, like Loeys-Dietz syndrome or vascular Ehlers-Danlos syndrome, you have a significantly higher risk of a thoracic aortic aneurysm and aortic or another blood vessel dissection or rupture.
- Bicuspid aortic valve – Nearly half of those who have an aortic valve with two cusps instead of three might develop an aortic aneurysm.
THORACIC AORTIC ANEURYSM COMPLICATIONS
Tears in the wall of the aorta and rupture of the aorta are the major complications of the thoracic aortic aneurysm. A ruptured aortic aneurysm could lead to life-threatening internal bleeding. In general, the bigger the aneurysm, the higher the risk of rupture.
Signs and symptoms that your thoracic aortic aneurysm has rupture include:
- Unexpected, intense, and persistent chest or back pain
- Pain that spreads to your back
- Difficulty breathing
- Low blood pressure
- Loss of consciousness
- Shortness of breath
- Trouble swallowing
- Weakness or paralysis of one side of the body, trouble speaking, or other signs of a stroke
Blood clot risk
An additional complication of aortic aneurysms is the risk of blood clots. Small blood clots could develop in the region of the aortic aneurysm. If a blood clot breaks loose from the inside wall of an aneurysm, it could block a blood vessel elsewhere in your body, possibly causing severe complications.
THORACIC AORTIC ANEURYSM DIAGNOSIS
Thoracic aortic aneurysms are usually found during routine medical tests, like a chest X-ray, CT scan, or ultrasound of the heart, sometimes ordered for a different reason.
Your doctor or primary care physician will ask questions about your signs and symptoms, as well as your family’s history of aneurysm or unexpected death.
If your doctor or primary care physician thinks that you have an aortic aneurysm, imaging tests could confirm it. Tests for thoracic aortic aneurysm include:
- Echocardiogram (ECG) – An echocardiogram (ECG) uses sound waves to capture real-time pictures of your heart and the ascending aorta. This test displays how well your heart chambers and valves are working. It might be used to diagnose thoracic aortic aneurysms and screen family members of those with thoracic aortic aneurysms.
In some cases, your doctor or primary care physician might recommend a transesophageal echocardiogram to better view the aorta. For this test, the sound waves are generated from a device that is gently guided down your esophagus. - Computed tomography (CT) – Computed tomography (CT) scan uses X-rays to create cross-sectional pictures of the body, including the aorta. It could detect the size and shape of an aneurysm. During a computed tomography (CT) scan, you lie on a table inside a doughnut-shaped X-ray machine. A dye, known as contrast, might be administered into a vein to help your arteries be more visible on the images.
One downside of the use of computed tomography (CT) scan in detecting and following aortic aneurysms is the exposure to radiation, especially for people who need frequent monitoring, like those with Marfan syndrome. Although, newer computed tomography (CT) scan techniques might be used to lower your radiation exposure. - Magnetic resonance imaging (MRI) – A magnetic resonance imaging (MRI) uses a magnetic field and radio waves to take pictures of the body. Magnetic resonance imaging (MRI) might be used to diagnose an aneurysm and determine its size and location. In this test, you lie down on a table that slides into the tunnel (magnet).
Doctors or primary care physicians might inject a dye into your vein to help your blood vessels to be more visible on pictures (magnetic resonance angiography). This test might be an alternative to computed tomography (CT) scans for people who require frequent monitoring of aneurysms, to lower their exposure to radiation.
Screening for thoracic aortic aneurysms
Conditions that cause a thoracic aortic aneurysm might run in families. Your doctor or primary care physician recommends screening if a first-degree relative like a parent, sibling, son, or daughter has Marfan syndrome or another condition that can cause a thoracic aortic aneurysm.
Tests used to screen for thoracic aortic aneurysms might include:
- Echocardiogram (ECG) – If an echocardiogram shows an enlarged aorta or an aneurysm, you will likely require another imaging test within six or twelve months to make sure it has not grown larger.
- Genetic testing – If you have a family history of aneurysm or another suspected genetic condition that increases your risk of thoracic aortic aneurysm, you might want to consider genetic testing. You might also want to consider genetic counseling before starting a family.
Thoracic Aortic Aneurysm
THORACIC AORTIC ANEURYSM TREATMENT
The goal of treatment is to stop your aneurysm from growing and to treat it before it dissects or ruptures. Depending on the size and growth rate of your thoracic aortic aneurysm, treatment might vary from watchful waiting (monitoring) to surgery.
Monitoring
If your thoracic aortic aneurysm is small, your doctor or primary care physician might recommend imaging tests to monitor the aneurysm, along with medication and management of other medical conditions.
Usually, you will have an echocardiogram (ECG), computed tomography (CT), or magnetic resonance angiography (MRA) scan at least six months after your aneurysm is diagnosed, and at regular follow-up examinations. How usually you have these tests done depends on the cause and size of the aneurysm, and how fast it is growing.
Medications
If you have high blood pressure or blockages in your arteries, your doctor or primary care physician will likely prescribe medications to reduce your blood pressure and cholesterol.
These medications can include:
- Beta-blockers – Beta-blockers reduce your blood pressure by slowing your heart rate. For people with Marfan syndrome, beta-blockers might lower how fast the aorta is widening. Instances of beta-blockers include metoprolol (Lopressor, Toprol-XL, Kapspargo Sprinkle), atenolol (Tenormin), and bisoprolol.
- Angiotensin II receptor blockers – Your doctor or primary care physician might also prescribe these medications if beta-blockers are not enough to control your blood pressure or if you cannot take beta-blockers. These medications are usually recommended for people who have Marfan syndrome even if they do not have high blood pressure. Instances of angiotensin II receptor blockers include losartan (Cozaar), valsartan (Diovan) and olmesartan (Benicar).
- Statins – These medications could help reduce your cholesterol, which could help reduce blockages in your arteries and lower your risk of aneurysm complications. Instances of statins include atorvastatin (Lipitor), lovastatin (Altoprev), simvastatin (Zocor, FloLipid), and others.
If you smoke or chew tobacco, it is crucial that you quit. Using tobacco could worsen your aneurysm.
Surgery
Surgery is usually recommended for thoracic aortic aneurysms about 1.9 to 2.4 inches (about 5 to 6 centimeters) and larger. If you have Marfan syndrome, another connective tissue disease (CTD), a bicuspid aortic valve or a family history of aortic dissection, your doctor or primary care physician might recommend surgery for smaller aneurysms because of the higher risk of aortic dissection.
Most people with a thoracic aortic aneurysm have open-chest surgery, but in some select cases, your doctor or primary care physician might determine you are a candidate for a less invasive repair known as endovascular surgery.
The type of surgery you have depends upon your condition and the location of your thoracic aortic aneurysm.
- Open-chest surgery – Open-chest surgery to repair a thoracic aortic aneurysm usually involves removing the damaged part of the aorta and replacing it with a synthetic tube (graft), which is sewn into place. It usually takes a month or more to completely recover from this procedure. If you have Marfan syndrome or other associated conditions, you might have aortic root replacement.
Your surgeon removes a part of your aorta and sometimes the aortic valve and replaces the section of the aorta with a graft. The aortic valve might be replaced with a mechanical or biological valve. If the valve is not removed, the surgery is known as valve-sparing aortic root repair. - Endovascular surgery – Doctors or primary care physicians attach a synthetic graft to the end of a thin tube that is inserted through an artery in your leg and threaded up into your aorta. The graft a woven tube covered by a metal mesh support is placed at the area of the aneurysm. Tiny hooks or pins keep the graft in place. The graft reinforces the weakened part of the aorta to stop the rupture of the aneurysm.
Recovery time is usually faster with this procedure than with open-chest surgery, but endovascular surgery cannot be done on everyone. Ask your doctor or primary care physician whether it is right for you. After endovascular surgery, you will require to have regular follow-up imaging scans to ensure that the graft is not leaking. - Emergency surgery – However, it is possible to repair a ruptured aortic aneurysm with emergency surgery, the risk is much higher and there is a greater risk of complications. Because of this, doctors or primary care physicians prefer to identify and treat thoracic aortic aneurysms before they rupture and to follow through with lifelong monitoring and appropriate preventive surgery.
If you or anyone you know is suffering from a thoracic aortic aneurysm, our expert providers at Specialty Care Clinics will take care of your health and help you recover.
Call(469) 545-9983 to book a telehealth appointment for an at-home check-up.
