WHAT IS PLANTAR FASCIITIS?
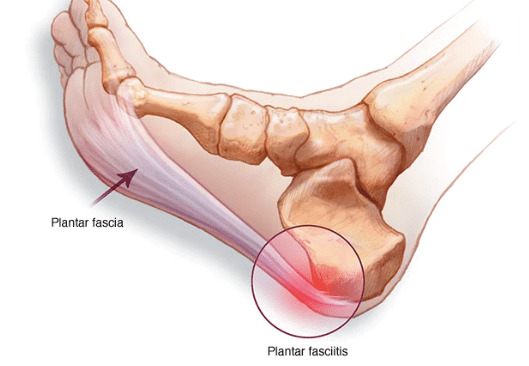
Plantar fasciitis is one of the most frequent causes of heel pain. It involves swelling of a thick band of tissue that runs across the bottom of your foot and joins your heel bone to your toes (plantar fascia).
Plantar fasciitis commonly causes stabbing pain that generally happens with your first steps in the morning. As you get up and move, the pain normally reduces, but it may return after long periods of standing or when you stand up after sitting.
Plantar fasciitis is more frequent in runners. People who are overweight and those who wear shoes with inadequate support also have a high risk of plantar fasciitis.
PLANTAR FASCIITIS SYMPTOMS
Plantar fasciitis generally causes a stabbing pain in the base of your foot near the heel. The pain is generally the worst with the first few steps after awakening, however, it could also be triggered by long periods of standing or when you get up after sitting. The pain is generally worse after exercise, not during it.
PLANTAR FASCIITIS CAUSES
Your plantar fascia is in the shape of a bowstring, supporting the arch of your foot and absorbing the impact when you walk. If the tension and stress on this bowstring become too great, small tears could happen in the fascia. Repeated stretching and tearing could irritate or inflame the fascia, however, the cause remains unclear in many cases of plantar fasciitis.
PLANTAR FASCIITIS RISK FACTORS
Even though plantar fasciitis could develop without an obvious cause, some factors could increase your risk of developing this condition. They include:
- Age – Plantar fasciitis is most common between the ages of 40 years and 60 years.
- Specific types of exercise – Activities that place a lot of stress on your heel and attached tissue for example long-distance running, ballet dancing, and aerobic dance could contribute to the beginning of plantar fasciitis.
- Foot mechanics – Flat feet, a high arch, or even an abnormal pattern of walking could affect the way weight is distributed when you are standing and could put added stress on the plantar fascia.
- Obesity – Excess pounds exert extra stress on the plantar fascia.
- Occupations that keep you on your feet – Factory workers, teachers, and others who spend most of their work hours walking or standing on hard surfaces could damage the plantar fascia.
PLANTAR FASCIITIS COMPLICATIONS
Ignoring plantar fasciitis might result in chronic heel pain that impedes your regular activities. Changing the way you walk as a way to ease plantar fasciitis pain may lead to foot, knee, hip, or back problems.
PLANTAR FASCIITIS DIAGNOSIS
Plantar fasciitis is diagnosed based on your medical history and physical exam. During the exam, your doctor or primary care physician will check for areas of tenderness in your foot. The location of your pain could help determine its cause.
Imaging tests
Usually, no tests are required. Your doctor or primary care physician may recommend an X-ray or magnetic resonance imaging (MRI) to make sure another problem, for example, a stress fracture, is not causing you pain.
Sometimes an X-ray shows a piece of bone protruding (spur) from the heel bone. In the past, these bone spurs were usually blamed for heel pain and removed surgically. But many people with bone spurs on their heels do not have heel pain.
PLANTAR FASCIITIS TREATMENT
Most people who have plantar fasciitis heal in several months with conservative treatment, including resting, icing the painful region, and stretching.
Medications
Pain relievers like ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve) might relieve the pain and inflammation caused by plantar fasciitis.
Therapies
Stretching and strengthening exercises or using special devices might relieve symptoms. They include:
- Physical therapy – A physical therapist could show you a series of exercises to stretch the plantar fascia and Achilles tendon and to strengthen lower leg muscles. A therapist may also teach you to apply athletic taping to support the base of your foot.
- Night splints – Your physical therapist or doctor or primary care physician may suggest that you wear a splint that stretches your calf and the arch of your foot while you sleep. This keeps the plantar fascia and Achilles tendon in a lengthened position overnight to promote stretching.
- Orthotics – Your doctor or primary care physician may prescribe off-the-shelf or custom-fitted arch supports (orthotics) to help distribute pressure to your feet more evenly.
Surgical or other procedures
If more conservative measures are not working after several months, your doctor or primary care physician may suggest:
- Injections – Injecting steroid medication into the tender region could provide temporary pain relief. Multiple shots are not suggested because they could weaken your plantar fascia and possibly cause it to rupture. Using ultrasound imaging, platelet-rich plasma obtained from the patient’s own blood could be administered to promote tissue recovery.
- Extracorporeal shock wave therapy – In this procedure, sound waves are directed at the region of heel pain to stimulate healing. It is generally used for chronic plantar fasciitis that has not responded to more conservative treatments. Some studies show promising results, but they have not always shown to be effective.
- Ultrasonic tissue repair – This is a minimally invasive technology. It uses ultrasound imaging to guide a syringe-like probe into the damaged plantar fascia tissue. Using ultrasound energy, the probe tip vibrates quickly to break up the damaged tissue, which is then suctioned out.
- Surgery – Few people require surgery to detach the plantar fascia from the heel bone. It is usually an option only when the pain is severe and other treatments have failed. It could be done as an open procedure or through a small incision with local anesthesia.
If you or anyone you know is suffering from plantar fasciitis, our expert providers at Specialty Care Clinics will take care of your health and help you recover.
Call 469-545-9983 to book an telehealth appointment for an at home check-up.